|
History > 2008 > USA > Health (IV)

Ramona Lamascola
with her mother, Theresa Lamascola.
Photograph: Ruby Washington
The New York Times
Doctors Say Medication Is Overused in Dementia
NYT
24.6.2008
https://www.nytimes.com/2008/06/24/health/24deme.html
Gene-Hunters Find Hope and Hurdles
in Schizophrenia Studies
July 31, 2008
The New York Times
By NICHOLAS WADE
Two groups of researchers hunting for schizophrenia genes on a
larger scale than ever before have found new genetic variants that point toward
a different understanding of the disease.
The variants discovered by the two groups, one led by Dr. Kari Stefansson of
Decode Genetics in Iceland and the other by Dr. Pamela Sklar of Massachusetts
General Hospital, are rare. They substantially increase the risk of
schizophrenia but account for a tiny fraction of the total number of cases.
This finding, coupled with the general lack of success so far in finding common
variants for schizophrenia, raises the possibility that the genetic component of
the disease is due to a large number of variants, each of which is very rare,
rather than to a handful of common variants.
“What is beginning to emerge is that a lot of the risk of brain diseases is
conferred by rare deletions,” Dr. Stefansson said. The three variants discovered
by his group and Dr. Sklar’s involve the deletion of large sections of DNA from
specific sites in a patient’s genome.
Their report, published online Wednesday by the journal Nature, follows a
finding in March from researchers at the University of Washington in Seattle
that rare deletions and duplications of DNA figure prominently in schizophrenia.
The new focus on rare mutations suggests that natural selection is highly
efficient at removing schizophrenia-causing genes from the population. Despite
selection against the disease, according to this new idea, schizophrenia
continues to appear because it is driven by a spate of new mutations that occur
all the time in the population.
“We’ve looked for common variants in schizophrenia and get almost nothing,” said
Dr. David Goldstein, a geneticist at Duke University and one of Dr. Stefansson’s
co-authors. “This means natural selection has done a really good job of purging
them away, and we’re left with rare variants, a constant flow of them, as the
principal driver of the disease.”
“This may be the case in other brain diseases, too,” Dr. Goldstein said,
“because successful cognitive functioning is a highly complex system and there
are many independent ways to take it down.”
One obvious way in which natural selection acts against the disease is that
schizophrenics have fewer children than others. “The brain diseases are those
where we find the biggest evidence for negative selection, “ Dr. Stefansson
said, a finding he found surprising because “I would have thought the brain was
a luxury organ when it comes to reproductive success.”
Devising treatments for schizophrenia could be more difficult if the disease is
caused by subsets of 2,000 rare variants, say, rather than by just 20 common
ones. But several experts said it was too early to know what mix of common and
rare variants may cause the disease and whether that might affect the search for
treatments.
The search for common variants in schizophrenia, however, has not been very
successful so far, though not for want of trying. There have been more than a
thousand studies, implicating 3,608 genetic variants.
But when all the data are pooled, only 24 of those variants turn out to be
statistically significant, according to an analysis in the current issue of
Nature Genetics by a group led by Dr. Lars Bertram of Massachusetts General
Hospital.
Most of the early studies had too few patients and focused on mutations in what
seemed to be plausible genes, an approach that is rarely successful. A new and
more fruitful method is to survey the whole genome without any prior
assumptions, a strategy made possible by new gene chips and a database of human
genetic variation known as the hapmap.
But even these genome-wide association studies have had little success in
finding common variants. Five such studies of schizophrenia have now been
completed, and one of the largest found no common variants, Dr. Bertram said.
The consortiums led by Dr. Stefansson and Dr. Sklar are still looking for common
variants but published their rare deletions now because they were so prominent,
Dr. Sklar said.
Should most of the genetic component of the disease turn out to depend on
multiple rare variants, the task of finding general treatments might seem to be
far harder than if a few common variants were involved. Dr. Stefansson said,
however, that was not the case.
“The only thing you need is to find pathways that are up- or down-regulated,” he
said. “The assumption that this is a more difficult situation is just not
correct.”
Dr. Thomas Insel, director of the National Institute of Mental Health, said the
new landscape might complicate development of genetic diagnostics for
schizophrenia but not necessarily of therapies.
“If you can understand the mechanism,” Dr. Insel said, “you should be able to
devise new treatments. So I think this is a big advance, not a signal for
hopelessness.”
Gene-Hunters Find
Hope and Hurdles in Schizophrenia Studies, NYT, 31.7.2008,
http://www.nytimes.com/2008/07/31/health/research/31gene.html
U.S. Blacks, if a Nation,
Would Rank High on AIDS
July 30, 2008
The New York Times
By LAWRENCE K. ALTMAN
If black America were a country, it would rank 16th in the world in the
number of people living with the AIDS virus, the Black AIDS Institute, an
advocacy group, reported Tuesday.
The report, financed in part by the Ford Foundation and the Elton John AIDS
Foundation, provides a startling new perspective on an epidemic that was first
recognized in 1981.
Nearly 600,000 African-Americans are living with H.I.V., the virus that causes
AIDS, and up to 30,000 are becoming infected each year. When adjusted for age,
their death rate is two and a half times that of infected whites, the report
said. Partly as a result, the hypothetical nation of black America would rank
below 104 other countries in life expectancy.
Those and other disparities are “staggering,” said Dr. Kevin A. Fenton, who
directs H.I.V. prevention efforts at the Centers for Disease Control and
Prevention, the federal agency responsible for tracking the epidemic in the
United States.
“It is a crisis that needs a new look at prevention,” Dr. Fenton said.
In a separate report on Tuesday, the United Nations painted a somewhat more
optimistic picture of the worldwide AIDS epidemic, noting that fewer people are
dying of the disease since its peak in the late 1990s and that more people are
receiving antiretroviral drugs.
Nevertheless, the report found that progress remained uneven and that the future
of the epidemic was uncertain. The report was issued in advance of the 17th
International AIDS Conference, which begins this weekend in Mexico City.
The gains are partly from the Bush administration’s program to deliver drugs and
preventive measures to people in countries highly affected by H.I.V.
The Black AIDS Institute took note of that program in criticizing the
administration’s efforts at home. The group said that more black Americans were
living with the AIDS virus than the infected populations in Botswana, Ethiopia,
Guyana, Haiti, Namibia, Rwanda or Vietnam — 7 of the 15 countries that receive
support from the administration’s anti-AIDS program.
The international effort is guided by a strategic plan, clear benchmarks like
the prevention of seven million H.I.V. infections by 2010 and annual progress
reports to Congress, the group said. By contrast, it went on, “America itself
has no strategic plan to combat its own epidemic.”
In a telephone interview, Dr. Fenton said, “We recognize this is a crisis, and
clearly more can be done.”
The institute, based in Los Angeles, describes itself as the only national
H.I.V./AIDS study group focused exclusively on black people. Phill Wilson, the
group’s chief executive and an author of the report, said his group supported
the government’s international anti-AIDS program. But Mr. Wilson’s report also
said that “American policy makers behave as if AIDS exists ‘elsewhere’ — as if
the AIDS problem has been effectively solved” in this country.
The group also chided the government for not reporting H.I.V. statistics to the
United Nations for inclusion in its biannual report.
Dr. Fenton said the C.D.C. had ensured that its data were forwarded to officials
in the Department of Health and Human Services and was investigating why the
data were not in the United Nations report.
Others speaking for the agency said the answer would have to come from the State
Department, which did not respond to an inquiry.
Dr. Helene Gayle, president of CARE and a former director of H.I.V. prevention
efforts at the disease control centers, told reporters on Tuesday that the
United States needed to devote more resources to care for people with sexually
transmitted diseases. Such infections can increase the risk of H.I.V. infection.
The federal government and communities needed to promote more testing among all
people, particularly blacks, to detect H.I.V. infection in its earliest stages
when treatment is more effective, Dr. Gayle said.
Also, she said, more needed to be done to promote needle exchange programs,
which have proved effective in preventing H.I.V. infection among injecting drug
users but that are illegal in many places.
The United Nations report said that in Rwanda and Zimbabwe, changes in sexual
behavior had led to declines in the number of new H.I.V. infections.
Condom use is increasing among young people with multiple partners in many
countries and more young people are postponing their initial sexual intercourse
before age 15.
The percentage of pregnant women receiving antiretroviral drugs to prevent
transmission of H.I.V. to their infants increased to 33 percent in 2007 from 14
percent in 2005. During the same period, the number of new infections among
children fell to 370,000 from 410,000.
The United Nations report affirmed treatment gains in Namibia, which increased
treatment to 88 percent of the estimated need in 2007, from 1 percent in 2003;
and in Cambodia, where the percentage rose to 67 in 2007 from 14 percent in
2004. Other countries with high treatment rates are Botswana, Brazil, Chile,
Costa Rica, Cuba and Laos.
In most areas of the world, more women than men are receiving antiretroviral
therapy, the report said.
Despite inadequate monitoring systems in many countries, data suggest that most
of the H.I.V. epidemics in the Caribbean appear to have stabilized. A few have
declined in urban areas in the Dominican Republic and Haiti which have had the
largest epidemics in the region.
Increased treatment was partly responsible for a decline in AIDS-related deaths
to an estimated 2 million in 2007 from 2.2 million in 2005.
The AIDS epidemic has had less overall economic effect than earlier feared, the
report said, but is having profound negative effects in industries and
agriculture in high-prevalence countries.
The United Nations has set 2015 as the year by which it hopes to reverse the
epidemic. But even if the world achieved that goal, the report said, “the
epidemic would remain an overriding global challenge for decades.”
To underscore the point, the United Nations said that for every two people who
received treatment, five people became newly infected.
U.S. Blacks, if a
Nation, Would Rank High on AIDS, NYT, 30.7.2008,
http://www.nytimes.com/2008/07/30/health/research/30aids.html
The Price of Beauty
As Doctors Cater to Looks,
Skin Patients Wait
July 28, 2008
The New York Times
By NATASHA SINGER
Dr. Donald Richey, a dermatologist in Chico, Calif., has two office telephone
numbers: calls to the number for patients seeking an appointment for skin
conditions like acne and psoriasis often go straight to voice mail, but a
full-time staff member fields calls on the dedicated line for cosmetic patients
seeking beauty treatments like Botox.
Dr. Richey has two waiting rooms. The medical patients’ waiting room is
comfortable, but the lounge for cosmetic clients is luxurious, with soft music
and flowers.
And he has two kinds of treatment rooms: clinical-looking for skin disease
patients, soothing for cosmetic laser patients.
“Cosmetic patients have a much more private environment than general medical
patients because they expect that,” said Dr. Richey, who estimated that he spent
about 40 percent of his time treating cosmetic patients. “We are a little bit
more sensitive to their needs.”
Like airlines that offer first-class and coach sections, dermatology is fast
becoming a two-tier business in which higher-paying customers often receive
greater pampering. In some dermatologists’ offices, freer-spending cosmetic
patients are given appointments more quickly than medical patients for whom
health insurance pays fixed reimbursement fees.
In other offices, cosmetic patients spend more time with a doctor. And in still
others, doctors employ a special receptionist, called a cosmetic concierge, for
their beauty patients.
Dr. David M. Pariser, a dermatologist in Norfolk, Va., and the president-elect
of the American Academy of Dermatology, said some practices did maintain
preferential policies for cosmetic patients.
“The message is that the cosmetic patient is more important than the medical
patient, and that’s not a good message,” Dr. Pariser said.
At a time when dermatologists are trying to advance the idea of a national skin
cancer epidemic, such a two-tier system is raising concerns that the coddling of
beauty patients may divert attention from skin diseases.
A study published last year in The Journal of the American Academy of
Dermatology found that dermatologists in 11 American cities and one county
offered faster appointments to a person calling about Botox than for someone
calling about a changing mole, a possible sign of skin cancer.
And dermatologists nationwide are increasingly hiring nurse practitioners and
physicians’ assistants, called physician extenders, who primarily see medical
patients, according to a study published earlier this year in the same journal.
“What are the physician extenders doing? Medical dermatology,” Dr. Allan C.
Halpern, chief of dermatology at Memorial Sloan-Kettering Cancer Center in
Manhattan, said in a melanoma lecture at a dermatology conference this year.
“What are the dermatologists doing? Cosmetic dermatology.”
There are no published studies showing that the rise of beauty procedures has
caused harm to medical dermatology patients. If patients with skin problems have
difficulty getting appointments, it is because over the last 30 years the demand
to see skin doctors has far outstripped the number of physicians trained in the
specialty, said Dr. Jack S. Resneck Jr., an assistant professor of dermatology
at the medical school of the University of California, San Francisco.
Dr. Resneck, who researches professional issues in dermatology, said about
10,500 dermatologists now practiced in the United States, the majority devoting
little time to vanity medicine.
Even so, dermatologists perform several million beauty treatments annually,
according to estimates by the American Society for Dermatologic Surgery,
including more than two million anti-wrinkle injection treatments last year — an
increase of 130 percent over 2005.
Several patients interviewed for this article said that they believed the
dermatologists they visited for medical care treated them as potential cosmetic
consumers. Dianne Ryan, who works for an airline in Dallas, went to a
dermatologist in her insurance network three years ago after her husband pointed
out a mole growing on the side of her foot, she said. The doctor dismissed the
mole as benign, she said, but recommended she buy his brand of bleaching cream
for pigmentation on her face.
A few months later, Ms. Ryan said, she sought a second opinion from another
dermatologist, whose diagnosis was melanoma.
“I don’t know if dermatology, with all the new technology, is turning away from
melanoma or whether it is the glamour and excitement,” said Ms. Ryan, who was
called by this reporter after an exchange in a chat room of the Melanoma
Research Foundation. “If you do an extreme makeover on someone, you are a hero.”
Dermatology is one of the fields — along with plastic surgery and behavioral
sleep medicine — in which patients are not only willing to pay for
quality-of-life treatments that may not be covered by insurance, but also
willing to pay much more for such treatments than insurers would pay for a
medical procedure that takes a similar amount of time.
Some health insurers reimburse a doctor $60 to $90 for a visit including a
full-body skin cancer check that might take 10 minutes; for Botox injections to
the forehead, a doctor might receive $500 for 10 minutes, paid on the day of
treatment.
According to a presentation for doctors from Allergan, the makers of Botox, a
medical dermatology practice might have a net income of $387,198 annually, but a
dermatologist who decreased focus on skin diseases while adding cosmetic medical
procedures to a practice could net $695,850 annually. The same material advises
doctors to “identify and segment high priority customers.”
People who wish to avoid a cosmetic-driven practice should simply seek
appointments with medical dermatologists who focus on skin diseases, said Dr.
Alexa B. Kimball, the vice chairwoman of dermatology at Massachusetts General
Hospital in Boston.
But many dermatologists now offer both medical treatment and beauty procedures,
which can confuse patients. And some doctors differentiate between patients —
either within their own practices or by treating cosmetic patients in
stand-alone facilities called medical spas.
Lecturers at the annual meeting of the American Academy of Dermatology, held in
San Antonio in February, encouraged such segregation.
For example, Dr. Jason R. Lupton, a dermatologist in Del Mar, Calif., advised
young physicians to oblige cosmetic patients by giving them appointments within
seven days; empty appointment slots could later be filled with general
dermatology patients, he said.
In a follow-up telephone interview, Dr. Lupton said that, in his own practice,
he accommodated medical and cosmetic patients equally.
In an interview, Dr. Susan H. Weinkle, a dermatologist in Bradenton, Fla., said
that she typically spends more time with cosmetic patients because they come in
wanting to look better, the kind of amorphous desire that takes longer to
satisfy than defined medical problems. One of her staff members always calls a
beauty client to follow up, she said.
“It is very rare that you would call an acne patient and say, ‘How are you doing
with that new prescription?’ ” Dr. Weinkle said. “But with a cosmetic patient,
the consultant calls them the next day.”
This dual-class treatment system is not limited to the fanciest of private
practices. Even academic institutions like the University of Michigan Health
System in Ann Arbor are openly catering to beauty consumers. The Web site of the
dermatology department warns a medical patient seeking an appointment to obtain
a referral from a primary care physician “regardless of your type of insurance.”
Meanwhile, the same Web site —
www.med.umich.edu/derm/patient/cdlcappointment.shtml — promotes the
attentiveness of its cosmetic doctors and encourages those seeking vanity
procedures to ask about the “convenient” valet parking.
A new profession — called aesthetic practice consultant — has emerged to advise
doctors in the care of cosmetic patients.
“Instead of laying on an exam table with a paper liner, you have them lay on a
sheet,” said Deborah Bish, a former nurse who works as a practice consultant in
Yardley, Pa. “You have to class it up for these patients.”
It makes economic sense that dermatologists competing for Botox dollars want to
create enticing environments, said Julie Cantor, a lawyer and medical school
graduate who teaches a course in medical ethics at the law school of the
University of California, Los Angeles. But Ms. Cantor said research was needed
to determine whether such environmental changes alter a doctor’s behavior with
medical patients.
“If you really started treating patients differently based on their ability to
pay out of pocket, that’s a real problem,” Ms. Cantor said. “People who want
their wrinkles fixed to go to a wedding should not be treated better than those
who have psoriasis.”
Dr. Richey, the Chico, Calif., dermatologist, said that in his practice, the
attention to cosmetic patients had no bearing on the treatment of medical
patients; he maintains daily walk-in slots for medical patients with urgent skin
problems, and many of his patients visit both sides of his practice.
“I don’t believe in differentiating,” Dr. Richey said.
Nonetheless, some medical patients said that they believed other dermatologists
brushed off their medical concerns in favor of marketing cosmetic procedures.
Melissa Bundy, a health communications manager in Atlanta, said that several
years ago she went to a dermatologist who seemed more interested in selling face
treatments than in conducting a thorough skin cancer examination. She has since
switched doctors.
“Cosmetic things, it’s a really great business,” Ms. Bundy said. “But it really
does seem to be at the expense of people like me getting the medical services
that we are looking for.”
As Doctors Cater to
Looks, Skin Patients Wait, NYT, 28.7.2008,
http://www.nytimes.com/2008/07/28/us/28beauty.html
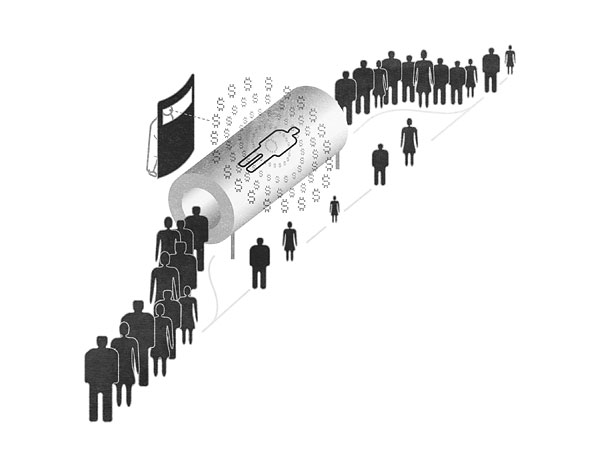
Illustration: John Hersey
Paying Doctors to Ignore Patients
NYT
24.7.2008
http://www.nytimes.com/2008/07/24/opinion/24bach.html
Op-Ed Contributor
Paying Doctors to
Ignore Patients
July 24, 2008
The New York Times
By PETER B. BACH
THE longstanding push-pull between Medicare and Congress has erupted again.
Last week, Congress, overriding a presidential veto, canceled Medicare’s
scheduled 10.6 percent cut in payment rates for doctors, and instead raised the
rates 1.1 percent. But this action fails to address the problem with the
Medicare payment system, which is not the amounts doctors are paid but the way
their payments are calculated.
Medicare pays doctors for specific services. If a patient has a checkup that
includes an X-ray, a urine analysis and a physical, Medicare pays the doctor
three separate fees.
Each fee is meant to reimburse the doctor for the time and skill he or she
devotes to the patient. But it is also supposed to pay for overhead, and this is
where the problem begins. To Medicare, a doctor’s overhead (or “practice
expense”) includes such items as rent, staff salaries and the cost of high-tech
medical equipment. When the agency pays a fee to a doctor who has performed a CT
scan, it is meant to cover some of the cost of buying or leasing the scanner
itself. Services using more expensive equipment generate higher fees.
Any first-year business school student can see the profit opportunity here. The
cost of a CT scanner is fixed, but a doctor earns fees each time it is used.
This means that a scanner becomes highly profitable as soon as it’s paid for.
In contrast, the doctor-patient visit, which involves no expensive equipment,
offers no significant profit opportunity. So the best way for a doctor to make
money in his practice is not to spend time with patients but to use equipment as
much as possible. That means moving the maximum number of patients through the
practice, and spending the minimum amount of time with each one.
From 2000 to 2005, the number of Medicare patients seen by doctors increased by
8.5 percent, while the number of services each one received was up 14 percent,
according to the Government Accountability Office.
It’s not only Medicare that pays doctors on a fee-for-service basis; most
private insurers do also. This is part of the reason that spending on physician
services nationwide has risen every year since 2000 by about $25 billion. This
year the tab will exceed $500 billion.
Doctors who do their own CT scanning and other imaging order roughly two to
eight times as many imaging tests as those who do not have their own equipment,
a 2002 study by researchers at the University of North Carolina found.
Altogether, doctors are ordering roughly $40 billion worth of unnecessary
imaging each year — which adds up to nearly 2 percent of the total Americans pay
for health care.
No wonder the Government Accountability Office last month urged Medicare to find
a way to constrain doctors’ use of imaging tests.
Over the years, Congress and Medicare have made various attempts to stamp out
some of the most egregious excesses in Medicare payments. Sometimes they have
succeeded. In 2004 and 2005, when Congress lowered the fees associated with
anti-testosterone drugs used to treat prostate cancer, urologists and other
doctors prescribed them less.
Around the same time, though, urologists started buying multimillion-dollar
radiation therapy machines for treating prostate cancer. Reimbursement for
radiation treatment remains very generous.
Clearly, scattershot strategies aimed at individual fees are unlikely to reduce
health care costs. More fundamental changes are needed in the way doctors are
paid.
For their time, doctors should be given a stipend for each of their patients. It
should be larger for patients with complicated medical conditions and smaller
for those who are healthy, and it should not be influenced by the number of
services or tests a doctor orders.
For overhead, doctors should be paid an amount that covers the typical cost of
tests and treatments needed to address a patient’s condition. This strategy —
known as “case rate” or “prospective” payment — is standard in American
hospitals. The hospital receives a payment for dealing with a patient’s
underlying condition rather than individual payments for each test and
treatment. This approach offers no incentive to run unneeded tests, and it has
been credited with substantially slowing the growth in Medicare payments to
hospitals.
Without changes to the way Medicare pays doctors, the fights in Congress over
raising or lowering payment rates will continue. And doctors will still have no
financial incentive to do what is most important: spend more time with their
patients.
Peter B. Bach, a doctor at Memorial Sloan-Kettering Cancer Center, was a senior
adviser to the administrator of the Centers for Medicare and Medicaid Services
from 2005 to 2006.
Paying Doctors to Ignore
Patients, NYT, 24.7.2008,
http://www.nytimes.com/2008/07/24/opinion/24bach.html
Billionaires Back Antismoking Effort
July 24, 2008
Yhe New York Times
By DONALD G. MCNEIL JR
Bill Gates and Mayor Michael R. Bloomberg announced on Wednesday that they
will spend $500 million to stop people around the world from smoking.
The World Health Organization estimates that tobacco will kill up to a billion
people in the 21st century, most of them in poor and middle-income countries. In
an effort to cut that number, Mr. Bloomberg’s foundation plans to commit $250
million over four years on top of $125 million he announced two years ago. The
Bill and Melinda Gates Foundation is allocating $125 million over five years.
That far outstrips current spending of about $20 million a year on antismoking
campaigns in poor and middle-income countries, according to a recent W.H.O.
report.
The $500 million would be spent on a multipronged campaign — nicknamed Mpower —
that Mr. Bloomberg and Dr. Margaret Chan, director of the health organization,
outlined in February. It coordinates efforts by the Bloomberg Initiative to
Reduce Tobacco Use, the health organization, the World Lung Foundation, the
Johns Hopkins Bloomberg School of Public Health, the Centers for Disease Control
and Prevention Foundation and the Campaign for Tobacco-Free Kids.
The campaign will urge governments to sharply raise tobacco taxes, outlaw
smoking in public places, outlaw advertising to children and free giveaways of
cigarettes, start antismoking advertising campaigns and offer their citizens
nicotine patches or other help quitting. Third world health officials, consumer
groups, journalists, tax officers and others will be brought to the United
States for workshops on topics like lobbying, public service advertising,
catching cigarette smugglers and running telephone hot lines for smokers wanting
to quit. A list of grants is at tobaccocontrolgrants.org.
The campaign will concentrate on five countries where most of the world’s
smokers live: China, India, Indonesia, Russia and Bangladesh.
Dr. Richard Peto, an Oxford epidemiologist who leads studies on the effects of
smoking in the developing world, called the announcement “excellent news.”
“I reckon this will avoid tens of millions of deaths in my lifetime and hundreds
of millions in my kids’ lifetimes,” he said.
Catherine Armstrong, a spokeswoman for British American Tobacco — one of the
Western tobacco companies that focuses on sales to the third world — would not
comment directly on the new initiative. But she said, “We have no problem with
government organizations educating people on the risks of tobacco.”
Mr. Bloomberg, founder of the financial news company bearing his name and
creator of the Bloomberg Family Foundation, has long been known for his
antipathy to tobacco. During his administration, New York has adopted several
antismoking measures, including a ban on smoking in bars and restaurants, and
significant increases in cigarette taxes. His foundation gave $2 million to the
W.H.O. to underwrite its latest tobacco report.
“When I announced this initiative, I said that I hoped that others would step
forward,” said Mr. Bloomberg, referring to his initial $125 million commitment,
in a written statement released before the afternoon news conference in Midtown
Manhattan. “I’m delighted Bill and Melinda Gates are supporting one of the most
important public health efforts of our time.”
It promises to be a struggle. Cigarettes are not only highly addictive and
supported by huge advertising campaigns, they are also an important source of
income for many foreign governments. In some countries, tobacco is a state-owned
monopoly, and low and middle-income countries collect $66 billion a year in
tobacco taxes.
About 5 percent of countries in the world have any antismoking measures like
those the campaign envisions.
But Dr. Peto said anti-smoking campaigns were already having effects in some
countries. He surveyed thousands of smokers in China in the 1990s — “before the
government was taking it seriously,” he said — and found 4 percent who
identified themselves as former smokers. In his more recent surveys, he said,
there were 20 percent.
In India, where people have long chewed tobacco but widespread smoking is more
recent, Dr. Peto said he found almost no one who had quit. “India is where China
was in the mid-1990s,” he said.
Waves of lung cancer deaths — which typically begin about 40 years after smoking
takes hold in a society — help persuade the next generation that smoking is
dangerous, as in the United States in the 1960s, he said. And, he added, “When
doctors and journalists start to take it seriously, things start to change.”
The Gates foundation’s main focus has been global health, but up until now it
has concentrated mostly on infectious diseases like AIDS, tuberculosis and
malaria rather than chronic ones like the cancers caused by tobacco. A
spokeswoman for the foundation said that some years ago, Mr. Gates read “The
Tobacco Atlas,” a 2002 publication from the World Health Organization describing
worldwide tobacco use — much of it by children. “He said, ‘Wow, why aren’t we
looking at this?’ ” said the spokeswoman, Melissa Derry.
Mr. Gates recently gave up his post as president of Microsoft to devote himself
full time to running the foundation, which has assets of about $37 billion.
Billionaires Back
Antismoking Effort, NYT, 24.7.2008,
http://www.nytimes.com/2008/07/24/health/24smoke.html?hp
Health Plan From Obama Spurs Debate
July 23, 2008
The New York Times
By KEVIN SACK
It is one of the most audacious promises in a campaign that
has been thick with them.
In speech after speech, Senator Barack Obama has vowed that he will lower the
country’s health care costs enough to “bring down premiums by $2,500 for the
typical family.” Moreover, Mr. Obama, the presumptive Democratic nominee, has
promised that his health plan will be in place “by the end of my first term as
president of the United States.”
Whether Mr. Obama can deliver is a matter of considerable dispute among health
analysts and economists. While there is consensus that the American health care
system is bloated with waste, eliminating enough to save $2,500 per family would
require simultaneous and synergistic solutions to a host of problems that have
proved intractable for decades.
Even if the next president and Congress can muster the political will, analysts
question whether significant savings would materialize in as little as four
years, or even in 10. But as Mr. Obama confronts an electorate that is deeply
unsettled by escalating health costs, he is offering a precise “chicken in every
pot” guarantee based on numbers that are largely unknowable. Furthermore, it is
not completely clear what he is promising.
His words about lowering “premiums” by $2,500 for the average family of four
have been fairly consistent. But the health policy advisers who formulated the
figure say it actually represents the average family’s share of savings not only
in premiums paid by individuals, but also in premiums paid by employers and in
tax-supported health programs like Medicare and Medicaid.
“What we’re trying to do,” said one of the advisers, David M. Cutler, in
explaining the gap between Mr. Obama’s words and his intent, “is find a way to
talk to people in a way they understand.”
The original arithmetic was somewhat basic. In May 2007, three Harvard
professors who are unpaid advisers to the Obama campaign — Mr. Cutler, David
Blumenthal and Jeffrey Liebman — produced a memorandum offering their “best
guess” that a menu of changes would produce savings of at least $200 billion a
year (it has since been revised to $214 billion). That would amount to about 8
percent of the $2.5 trillion in health care spending projected for 2009, when
the next president takes office.
The memorandum attributed specific savings to several broad initiatives, with
the numbers plucked from recent studies. Investments in computerized medical
records would save $77 billion a year, the advisers wrote. Reducing
administrative costs in the insurance industry would yield up to $46 billion.
Improving prevention programs and chronic disease management would be worth $81
billion.
The total savings were then divided by the country’s population, multiplied for
a family of four, and rounded down slightly to a number that was easy to grasp:
$2,500. The average cost of family coverage bought through an employer was
$12,106 in 2007, with workers paying $3,281 of that amount, according to the
Kaiser Family Foundation, a health research group.
Mr. Obama aspires to cover the country’s 47 million uninsured by requiring
insurers to accept all comers, regardless of their health status, and by
providing generous tax credits to low-income workers. The tax credits could be
used to buy into a new federal health plan or private plans marketed through a
government exchange.
The subsidies are expensive, estimated at well over $100 billion. Other
components of the Obama plan also bear up-front costs, like a pledge to spend
$50 billion over five years to speed the computerization of health records, $6
billion a year on tax credits to small businesses that provide coverage to
workers, and an unspecified amount to buffer businesses from high-cost insurance
claims.
The source Mr. Obama has identified to pay for them — the repeal of President
Bush’s tax cuts for those making more than $250,000 — would cover only about
half. That means additional health care savings would be needed, not only to
keep premiums under control but also to help pay for the subsidies.
A consensus has emerged among health economists that at least a third of the
country’s spending on health care is unnecessary. Both Mr. Obama, of Illinois,
and his Republican rival, Senator John McCain of Arizona, agree that significant
sums could be saved through reductions in unneeded procedures and improvements
in electronic record-keeping, prevention and chronic disease management.
But the dollar values Mr. Obama has attached to individual components of his
plan are beginning to attract scrutiny. In particular, the Congressional Budget
Office issued a report in May questioning the amount to be saved from the
computerization of health systems.
Mr. Obama took his estimate of $77 billion a year from a 2005 study by the RAND
Corporation (which cautioned that reductions of that magnitude would not emerge
for 15 years). The Congressional analysts found, however, that for various
methodological reasons the RAND study was “not an appropriate guide” to
potential savings.
This month, Mr. Obama’s health advisers tried to recast the debate so that the
questioning of any one number would not undermine the plan’s broader
credibility. They enlisted eight health policy experts to sign a letter that,
without endorsing the math behind any single initiative, proclaimed it was “not
only possible, but likely” that Mr. Obama could save $200 billion annually. They
did not say by when.
Mr. Cutler, who helped collect the signatures, said he and his colleagues had
decided “that our attempt to lay out one plausible scenario for the savings had
created more problems than it had solved.” He added: “Putting the debate where
this message puts it — do you believe we can save 8 percent of health spending
through a major series of public and private reforms — asks the question in a
way that is much more productive than the issue of ‘Do you believe a single
estimate among many, many studies?’ ”
Mr. Obama’s economic policy director, Jason Furman, said the campaign’s
estimates were conservative and asserted that much of the savings would come
quickly. “We think we could get to $2,500 in savings by the end of the first
term, or be very close to it,” Mr. Furman said.
The campaign won additional backing this week from Kenneth E. Thorpe of Emory
University, an authority on health care costs who helped formulate Bill
Clinton’s failed plan in 1993. In an assessment that he initiated in
coordination with the campaign, Mr. Thorpe wrote that if all of Mr. Obama’s
proposals were enacted they would reduce health spending by between $203 billion
and $273 billion by 2012. He calculated that half of the savings would accrue to
the federal government.
The Obama advisers said that while not all of the savings would translate into
lower premiums, consumers would gain in other ways. The savings to employers
would be passed along as higher wages, they predicted, and the savings to
government would eventually mean either lower taxes or added benefits.
But whether employers and governments respond that way cannot be guaranteed,
particularly in a difficult economy. And a number of health policy experts have
questioned whether the $2,500 projection is either fiscally or politically
realistic. Reducing health care costs, they emphasized, means taking money from
someone’s pocket and rationing care that Americans have come to expect, a recipe
for stiff resistance.
“There is no easy money because, as the saying goes, one person’s fraud and
abuse is another person’s income,” said Joseph R. Antos of the American
Enterprise Institute. “I wouldn’t think that four years or eight years or
probably 10 years will be enough to see numbers of that sort.”
The Commonwealth Fund, a health research group in New York, published a study in
December projecting that a robust overhaul consisting of 15 broad initiatives
would generate savings of only 6 percent after 10 years. “Doing it by the end of
a first term is ambitious and would require tough policies,” said Karen Davis,
the group’s president.
Jonathan B. Oberlander, who teaches health policy at the University of North
Carolina at Chapel Hill, called it wishful thinking. “Do they have the potential
to generate significant savings in the long run?” Dr. Oberlander asked. “Yes. Do
I believe they will produce substantial savings in the short run that can be
used to finance Obama’s plan? No.”
Health Plan From
Obama Spurs Debate, NYT, 23.7.2008,
http://www.nytimes.com/2008/07/23/us/23health.html?ref=opinion
Trial Intensifies Concerns About Safety of Vytorin
July 22, 2008
The New YorkTimes
By ALEX BERENSON
In a clinical trial, the cholesterol-lowering drug Vytorin did not help
people with heart-valve disease avoid further heart problems but did appear to
increase their risk of cancer, scientists reported Monday.
The scientists who reported on the trial, called Seas, cautioned against
panicking over the cancer findings, saying that even well-designed clinical
trials sometimes produce chance results. A review of two other, much larger
trials did not find a similar risk, they said.
Vytorin and Zetia, a companion drug, are prescribed each month to almost three
million people worldwide and are among the world’s top-selling medicines.
But other cardiologists and epidemiologists said that the cancer risk could not
be so easily dismissed.
The findings of the Seas trial will heighten concerns about Vytorin’s safety and
effectiveness, said Dr. Steven Nissen, a former president of the American
College of Cardiology and a longtime critic of Vytorin. Six months ago, a fourth
clinical trial, called Enhance, also failed to show that Vytorin benefited
patients, leading a panel of top cardiologists to recommend using Vytorin and
Zetia only as a last resort.
Since that recommendation, Vytorin and Zetia prescriptions have plunged, though
the drugs remain among the largest sellers for Merck and Schering- Plough, which
jointly sell them. The drugs had combined sales of $5 billion last year.
Shares of Merck and Schering skidded Monday after the Seas trial results were
reported, with Merck shares down 6 percent and Schering down 12 percent. After
the close of trading, both companies reported second-quarter earnings that were
slightly ahead of analysts’ estimates.
Vytorin is a single pill that combines two cholesterol-lowering medicines —
Zocor, or simvastatin, and Zetia, or ezetimibe. Both Zocor and Zetia are also
available as single pills. Zocor is a statin. Because two decades of research
have proven that statins reduce the risk of heart attacks and do not raise the
risk of cancer, the new safety concerns center around ezetimibe. In the United
States, about two million prescriptions a month are written for ezetimibe,
either independently as Zetia or in the Vytorin combination pill.
In the Seas trial, which involved nearly 1,900 patients whose heart valves were
partially blocked, participants were given either Vytorin or a placebo pill that
contained no medicine. Scientists hoped that the trial would show that patients
taking Vytorin would have a lower risk of needing valve replacement surgery or
having heart failure. But the drug did not show those benefits.
“No significant difference was observed between the treatment groups for the
combined primary endpoint,” Dr. Terje Pedersen, the principal investigator for
the study and a professor medicine at Ulleval University Hospital in Norway,
said. The primary endpoint is the result that scientists hope to prove when they
conduct a clinical trial.
However, patients taking Vytorin in the Seas trial did have a sharply higher
risk of developing and dying from cancer. In the trial 102 patients taking
Vytorin developed cancer, compared with 67 taking the placebo. Of those, 39
people taking Vytorin died from their cancer, compared with 23 taking placebo.
The absolute numbers of cancer cases were relatively small. But they reached
statistical significance, meaning the odds were less than 5 percent that they
were the result of chance.
To evaluate the cancer findings, Richard Peto, professor of medical statistics
and epidemiology at the University of Oxford, examined the interim results of
two other clinical trials of Vytorin — called Sharp and Improve-It. The
University of Oxford is leading the Sharp trial, which is sponsored by Merck and
Schering-Plough but run independently by the university’s Clinical Trial Service
Unit.
The Improve-It trial is being led by investigators by Harvard and Duke
University.
Both Sharp and Improve-It are comparing Vytorin with simvastatin — Zocor —
alone.
Neither trial has yet been completed, but the two trials combined have about
20,000 patients, nearly 10 times as many as the Seas trial.
So far, about the same number of patients taking Vytorin in Sharp and Improve-It
have developed cancer as those taking simvastatin alone, Mr. Peto said in London
on Monday. That fact strongly suggests that the finding in Seas is due to
chance, Mr. Peto said.
“I think we should not be diverted by fears of cancer,” he said.
Mr. Peto also noted that the increase in cancers was not clustered around a
single type of malignancy, but occurred widely. If ezetimibe did cause cancer,
it would be more likely to cause a single type than many types, he said.
But other doctors said the data from Improve-It and Sharp were not definitive.
The patients in those trials have generally been followed for one to two years,
while the Seas trial followed patients for four years. Because cancer generally
takes years to develop, it may take some time for Vytorin’s risks — if they are
real — to become evident in patients.
“I don’t know that you have much information about the cancer risk from the
other two trials,” said Dr. Bruce Psaty, professor of epidemiology at the
University of Washington.
In addition, the other two trials contain a puzzling finding. While the number
of cancer cases is similar in those trials among patients taking Vytorin and
those who were not, the number of cancer deaths is approximately one-third
higher among those taking Vytorin. In all, 136 people taking Vytorin have died
of cancer in the three trials, compared with 95 taking other medicines or a
sugar placebo pill.
Dr. Rob Califf, the director of the Duke Translational Medicine Institute and
the co-chairman of Improve-It, the largest of the clinical trials examining
Vytorin, said that stopping the trials early would be a mistake, since there was
no proof that ezetimibe — either in the form of Vytorin or Zetia — caused
cancer.
“To accept nonevidence as evidence is a worse mistake than to finish the trial
and get the data one way or the other,” Dr. Califf said. However, patients
outside the trials, who can choose to take other cholesterol-lowering drugs,
should discuss the findings with their doctors, he said. In general, patients
who can tolerate statins should take them and not ezetimibe, he said.
Trial Intensifies
Concerns About Safety of Vytorin, NYT, 22.7.2008,
http://www.nytimes.com/2008/07/22/business/22drug.html
Trying to Save by Increasing Doctors’ Fees
July 21, 2008
The New York Times
By MILT FREUDENHEIM
Cutting health costs by paying doctors more?
That is the premise of experiments under way by federal and state government
agencies and many insurers around the country. The idea is that by paying family
physicians, internists and pediatricians to devote more time and attention to
their patients, insurers and patients can save thousands of dollars downstream
on unnecessary tests, visits to expensive specialists and avoidable trips to the
hospital.
Nationally, Medicare and commercial insurers pay an average of only about $60 a
visit to the office of a primary-care doctor and rarely if ever pay for
telephone or e-mail consultations. Many health policy experts say the payments
are not enough to let the doctors spend more than a few minutes with each
patient.
Robert Williamson, a 60-year-old Philadelphia man, recalls the cursory exam he
received a few years ago from a harried doctor who, Mr. Williamson says, missed
the danger signals and sent him home. A short time later Mr. Williamson had a
stroke.
For want of a careful examination by a primary-care doctor, Mr. Williamson
became one of countless Americans each year whose unidentified or under-treated
illnesses escalate into medical conditions with catastrophic personal and
economic costs. Besides incurring $30,000 in hospital bills paid by his
employer’s insurer, Mr. Williamson had to stop working as a customer service
representative at Philadelphia Gas Works and go on Social Security disability,
at a current cost to taxpayers of $1,900 a month.
With Mr. Williamson’s new doctor, such an outcome would be much less likely.
“I give him my heart and diabetes readings by e-mail and phone, without getting
up out of my chair,” Mr. Williamson said. “I can get better directions, at the
very moment I need them. It’s life-saving.”
His current internist, Richard Baron, is one of more than 100 physicians in
metropolitan Philadelphia taking part in the experiment, which is being
conducted jointly by some of the region’s largest insurers. Dr. Baron still gets
a fee of only about $64 for each office visit. But his five-doctor group will
also receive $200,000 to $300,000 this year beyond their regular fees to keep
better track of their 8,400 patients.
“We are trying to do more e-mail care and telephone care, which we haven’t been
paid for in the past,” Dr. Baron said.
Insurers are conducting similar pilot projects in at least a half-dozen states,
in experiments involving thousands of doctors and nearly 2 million patients.
Many more are in the planning stages, at the urging of health policy experts and
employers that provide medical benefits.
The big government health care programs, Medicaid and Medicare, are also
studying the concept. A Medicaid experiment already under way in North Carolina
saved the government program in that state about $162 million in 2006. That was
11 percent less than the state would have spent under the old system of
reimbursement, according to an audit by Mercer, a consulting firm.
Earlier this month, as part of a bill to protect Medicare payments to doctors,
the Senate overrode President Bush’s veto to authorize $100 million to finance a
three-year Medicare pilot to further test the concept of spending more on
primary care.
Under the various payment experiments, family doctors are encouraged to hire
additional staff to help monitor patients’ treatment and follow-up, and to help
patients stay ahead of problems by sending reminders when they are due for
preventive tests like mammograms and colon exams.
For people like Mr. Williamson with serious chronic illnesses, the doctors take
personal charge, answering patients’ phone or e-mail questions promptly. In
emergencies, patients can show up at the office and see their doctors on short
notice.
Such features add up to a model of primary care that proponents refer to as
providing people with a “medical home” — a base where doctors, staff and
patients pull together as one big health-care family. Or at least that is the
ideal.
“It’s the latest new, new thing — testing whether medical homes can be a vehicle
for pulling America upwards from the grossly inefficient swamp in which our
health system is currently mired,” said Dr. Arnold Milstein, a senior consultant
at Mercer who is also member of the Medicare Payment Advisory Commission, an
independent Congressional agency.
The panel has recommended that Medicare expand its plans for a medical-home
pilot project next year that is expected to pay primary-care doctors in eight
states $30 to $40 a month extra for each person enrolled with a chronic illness.
In Michigan, the auto industry has been a major force behind one of the largest
medical-home projects yet devised. Blue Cross Blue Shield of Michigan, which has
4.7 million members, plans to spend $30 million this year to help primary-care
doctors offer such services. About 4,900 primary-care doctors are participating,
said Dr. Thomas Simmer, chief medical officer of Michigan Blue Cross.
Advocates of the approach hope it will attract more doctors to primary care.
Last year only 7 percent of medical school graduates chose family practice, a
field with a median income of $150,000, according to the American Academy of
Family Physicians. That compares with $406,000 for gastroenterologists and
$433,00 for cardiac surgeons, as measured by the Medical Group Management
Association.
The American Medical Association said that in its latest count, in 2006, there
were slightly more than 251,000 practicing family physicians, general,
practitioners, and internists in this country, compared with nearly 472,000
specialists.
“The pipeline of primary-care doctors has been running dry for several years,”
said Dr. Barbara Starfield, a health policy expert at Johns Hopkins University.
Many parts of the country do not meet the generally accepted standard of one
primary-care doctor for every 1,000 to 2,000 people, Dr. Starfield said.
The Philadelphia pilot project is sponsored by three of the area’s largest
insurers — Independence Blue Cross, Aetna and Cigna — as well as some local
providers of Medicaid services, which together have agreed to spend $13 million
on the program over the next three years.
Dr. Baron expects the project to add as much 15 percent to the annual revenue of
his medical group. He declined to specify the practice’s total gross income last
year, but said that each of the five physicians earned less than the $177,000
national median for internists.
To participate in the Philadelphia experiment, doctors must arrange for their
offices to keep in close communication with their entire rosters of patients.
Dr. Baron’s practice, besides the physicians, a business manager and clerical
assistants, has added a patient educator, whom he said would cost $60,000 in
salary plus $60,000 more for benefits and supporting technology. The group is
also spending $25,000 for part-time services of a data analyst.
Employers predict that better early care will reduce their health costs in the
long run. “We want to buy our care this way, we think it’s the right thing to
do,” said Dr. Paul Grundy, I.B.M.’s director of health care technology and
strategic initiatives.
Despite the hopes riding on the pilot projects, some experts are skeptical.
“There is very little concrete rigorous evidence that the medical home will do
all those wonderful things they want it to do,” said Mark Pauly, a health policy
economist at the Wharton School of the University of Pennsylvania.
Even executives at Aetna and Cigna are cautious about betting on a payoff from
the Philadelphia project, which was orchestrated by Pennsylvania’s Democratic
Governor Edward G. Rendell and his office of health care reform.
It is uncertain whether there will be a direct return on the investment within a
“reasonable time horizon,” said Dr. Don Liss, an Aetna medical director who is
an internist himself. Still, Dr. Liss added, “a reasonable body of evidence
suggests that improving primary care as a foundation for health care will
improve quality and access to care.”
The Pennsylvania program will start expanding to other parts of the state this
fall. It comes none too soon, in the view of Dr. Joseph Mambu, a family
physician in Lower Gwynedd, a Philadelphia suburb. Trying to build a
medical-home practice before the pilot project began, Dr. Mambu said he went
into debt installing an electronic medical records system and establishing
patient-friendly features like evening and Saturday office hours.
“Last year, I hit the red ink because of all the technology,” he said. “Unless
we get help from the insurance companies and the government, the system is going
down the toilet.”
But with the new medical-home money, Dr. Mambu said he expected to pay down his
debts and start a patient wellness program. The insurance pilot project, he
said, offers “a ray of hope.”
Trying to Save by
Increasing Doctors’ Fees, NYT, 21.7.2008,
http://www.nytimes.com/2008/07/21/business/21medhome.html?hp
While the U.S. Spends Heavily on Health Care, a Study Faults the Quality
July 17, 2008
The New York Times
By REED ABELSON
American medical care may be the most expensive in the world, but that does
not mean it is worth every penny. A study to be released Thursday highlights the
stark contrast between what the United States spends on its health system and
the quality of care it delivers, especially when compared with many other
industrialized nations.
The report, the second national scorecard from this influential health policy
research group, shows that the United States spends more than twice as much on
each person for health care as most other industrialized countries. But it has
fallen to last place among those countries in preventing deaths through use of
timely and effective medical care, according to the report by the Commonwealth
Fund, a nonprofit research group in New York.
Access to care in the United States has worsened since the fund’s first report
card in 2006 as more people — some 75 million — are believed to lack adequate
health insurance or are uninsured altogether. And within the nation, the report
found, the cost and quality of care vary drastically.
The findings are likely to provide supporting evidence for the political notion
that the nation’s health care system needs to be fixed. Both presumptive
presidential nominees, Senator John McCain and Senator Barack Obama, argue that
the country needs to get more value for its health care money, even if they do
not agree on what changes would be most effective. But few people these days
defend the status quo.
“It’s harder to keep deluding yourself or be complacent that we don’t have areas
that need improvement,” said Karen Davis, president of the Commonwealth Fund.
The study, which assesses the United States on 37 health care measures, finds
little improvement since the last report, as the cost of health care continues
to rise steadily and more people — even those with insurance — struggle to pay
their medical bills.
“The central finding is that access has deteriorated,” Ms. Davis said.
Even some experts who are quick to point to some of the country’s medical
successes, as in reducing the deaths from heart disease or childhood cancers,
for example, also acknowledge the need for change.
“We need to generate better value in this country,” said Dr. Denis A. Cortese,
the chief executive of the Mayo Clinic.
In some cases, the nation’s progress was overshadowed by improvements in other
industrialized countries, which typically have more centralized health systems,
which makes it easier to put changes in place.
The United States, for example, has reduced the number of preventable deaths for
people under the age of 75 to 110 deaths for every 100,000 people, compared with
115 deaths five years earlier, but other countries have made greater strides. As
a result, the United States now ranks last in preventable mortality, just below
Ireland and Portugal, according to the Commonwealth Fund’s analysis of World
Health Organization data. The leader by that measure is France, followed by
Japan and Australia.
Other countries worked hard to improve, according to the Commonwealth Fund
researchers. Britain, for example, focused on steps like improving the
performance of individual hospitals that had been the least successful in
treating heart disease. The success is related to “really making a government
priority to get top-quality care,” Ms. Davis said.
The presidential candidates both emphasize the need to shift the country’s
health priorities, to provide more medical care that helps prevent people from
developing disease and that helps control conditions before they become
expensive and hard to treat. And the mounting evidence indicates that such
issues are not simply political talking points, said Len Nichols, a health
economist at New America Foundation, a nonprofit group in Washington that
advocates universal health care coverage.
More hospital executives and doctors understand their performance could be
better, Mr. Nichols said.
Dr. James J. Mongan, the chief executive of Partners HealthCare System, a big
medical network in Boston, agrees that “there’s substantial room for
improvement.” Dr. Mongan is one of several health care leaders who is working
with the Commonwealth Fund to develop a model for a better system.
Business leaders also see a pressing need for health care changes, said Helen
Darling, the president of the National Business Group on Health, which
represents big employers that provide medical benefits to their workers. The
report “documents that it’s been as bad as we have been thinking it is,” she
said.
But Ms. Darling and others were also heartened because some areas in the report
said that the United States had shown marked improvement, including the
measurements hospitals use to track how well they treated conditions like heart
failure and pneumonia.
“It proves once again if you have quantitative information and metrics and make
people pay attention, they change,” Ms. Darling said.
But the report also emphasizes the inefficiencies of the American health care
system. The administrative costs of the medical insurance system consume much
more of the current health care dollar, about 7.5 percent, than in other
countries.
Bringing those administrative costs down to the level of 5 percent or so as in
Germany and Switzerland, where private insurers play a significant role, would
save an estimated $50 billion a year in the United States, Ms. Davis said.
“It kind of dwarfs everything else you can do,” she said.
Much of the high costs are attributed to the lack of computerized systems that
may link pharmacies and doctors’ offices for filling prescriptions, for example,
or that may enable insurers to more efficiently pay doctors’ bills.
“An awful lot of the waste in this system is the antiquity of the information
technology,” Ms. Darling said.
Karen Ignagni, the chief executive of America’s Health Insurance Plans, an
industry trade group, argues that much of the higher administrative costs stem
from the additional services provided by United States insurers, like disease
management programs, and the burdensome regulatory and compliance costs of doing
business in 50 states. A more uniform system could result in savings, she said.
While the U.S. Spends
Heavily on Health Care, a Study Faults the Quality, NYT, 17.7.2008,
http://www.nytimes.com/2008/07/17/business/17health.html
Op-Ed Columnist
The Luxurious Growth
July 15, 2008
The New York Times
By DAVID BROOKS
We all know the story of Dr. Frankenstein, the scientist so caught up in his
own research that he arrogantly tried to create new life and a new man. Today,
if you look at people who study how genetics shape human behavior, you find a
collection of anti-Frankensteins. As the research moves along, the scientists
grow more modest about what we are close to knowing and achieving.
It wasn’t long ago that headlines were blaring about the discovery of an
aggression gene, a happiness gene or a depression gene. The implication was
obvious: We’re beginning to understand the wellsprings of human behavior, and it
won’t be long before we can begin to intervene to enhance or transform human
life.
Few talk that way now. There seems to be a general feeling, as a Hastings Center
working group put it, that “behavioral genetics will never explain as much of
human behavior as was once promised.”
Studies designed to link specific genes to behavior have failed to find anything
larger than very small associations. It’s now clear that one gene almost never
leads to one trait. Instead, a specific trait may be the result of the interplay
of hundreds of different genes interacting with an infinitude of environmental
factors.
First, there is the complexity of the genetic process. As Jim J. Manzi pointed
out in a recent essay in National Review, if a trait like aggressiveness is
influenced by just 100 genes, and each of those genes can be turned on or off,
then there are a trillion trillion possible combinations of these gene states.
Second, because genes respond to environmental signals, there’s the complexity
of the world around. Prof. Eric Turkheimer of the University of Virginia,
conducted research showing that growing up in an impoverished environment harms
I.Q. He was asked what specific interventions would help children realize their
potential. But, he noted, that he had no good reply. Poverty as a whole has this
important impact on people, but when you try to dissect poverty and find out
which specific elements have the biggest impact, you find that no single factor
really explains very much. It’s possible to detect the total outcome of a
general situation. It’s harder to draw a linear relationship showing cause and
effect.
Third, there is the fuzziness of the words we use to describe ourselves. We talk
about depression, anxiety and happiness, but it’s not clear how the words that
we use to describe what we feel correspond to biological processes. It could be
that we use one word, depression, to describe many different things, or perhaps
depression is merely a symptom of deeper processes that we’re not aware of. In
the current issue of Nature, there is an essay about the arguments between
geneticists and neuroscientists as they try to figure out exactly what it is
that they are talking about.
The bottom line is this: For a time, it seemed as if we were about to use the
bright beam of science to illuminate the murky world of human action. Instead,
as Turkheimer writes in his chapter in the book, “Wrestling With Behavioral
Genetics,” science finds itself enmeshed with social science and the humanities
in what researchers call the Gloomy Prospect, the ineffable mystery of why
people do what they do.
The prospect may be gloomy for those who seek to understand human behavior, but
the flip side is the reminder that each of us is a Luxurious Growth. Our lives
are not determined by uniform processes. Instead, human behavior is complex,
nonlinear and unpredictable. The Brave New World is far away. Novels and history
can still produce insights into human behavior that science can’t match.
Just as important is the implication for politics. Starting in the late 19th
century, eugenicists used primitive ideas about genetics to try to re-engineer
the human race. In the 20th century, communists used primitive ideas about
“scientific materialism” to try to re-engineer a New Soviet Man.
Today, we have access to our own genetic recipe. But we seem not to be falling
into the arrogant temptation — to try to re-engineer society on the basis of
what we think we know. Saying farewell to the sort of horrible social
engineering projects that dominated the 20th century is a major example of human
progress.
We can strive to eliminate that multivariate thing we call poverty. We can take
people out of environments that (somehow) produce bad outcomes and try to
immerse them into environments that (somehow) produce better ones. But we’re not
close to understanding how A leads to B, and probably never will be.
This age of tremendous scientific achievement has underlined an ancient
philosophic truth — that there are severe limits to what we know and can know;
that the best political actions are incremental, respectful toward accumulated
practice and more attuned to particular circumstances than universal laws.
Bob Herbert is off today.
The Luxurious Growth,
NYT, 15.7.2008,
http://www.nytimes.com/2008/07/15/opinion/15brooks.html?ref=opinion
Individual health policies leave many behind
16 July 2008
USA Today
By Julie Appleby
Soon after a pediatrician noted in his medical records that 5-year-old Logan
Swaim was short for his age, his mother, Theresa, tried to buy health insurance.
Her husband, William, had started his own landscaping business after being
laid off, and the insurance he got from his former employer was about to expire.
Two insurers accepted the Swaims and three of their children for new coverage,
but they rejected Logan, fearing his height — 40½ inches — might indicate a
glandular problem that could be expensive to treat.
For two years, the Swaims paid all of Logan's medical bills themselves, about
$4,300. Eventually they got test results showing there was nothing wrong with
him. Even so, the insurers wouldn't cover him, Theresa Swaim says, because the
time to appeal the denial of coverage had expired.
Like the Swaims, nearly 18 million people nationwide buy their own insurance
because they're self-employed, are students or have jobs that don't offer
coverage. The so-called individual health insurance market works well for some,
but as the Swaims' case shows, it is fraught with complexities for many others.
Unlike group plans offered by employers — which provide coverage to everyone, no
matter how sick — there is no guarantee in most states that individuals can get
insurance. Even if they can, their policies may not cover existing medical
conditions such as hay fever, depression or pregnancy.
Fixing the problems in the individual market could go a long way toward
expanding health coverage in America, where 47 million people are uninsured.
State and federal lawmakers — and the presidential candidates — propose changes
that could reshape that market. One approach would loosen regulations, which
could prompt insurers to offer a wider range of plans to more people. The other
would increase government oversight to make it easier for people with health
conditions to get coverage.
Among recent developments:
• In the past few months, regulators in California, Connecticut and several
other states have fined or taken other action against insurers who revoked
individual coverage after policyholders fell ill, leaving them with thousands of
dollars in unpaid medical bills.
• In Congress, Sens. Ron Wyden, D-Ore., and Bob Bennett, R-Utah, are pushing the
first sweeping, bipartisan health care proposal in years, one that could shift
many workers from getting coverage through employers to buying their own
insurance. Breaking the link between employment and insurance, they say, would
let people keep their coverage when they lose or switch jobs. The proposal
requires everyone to have coverage and forces insurers to sell to all
applicants.
• Both presidential candidates say they want to improve options for people who
buy their own coverage. Democrat Barack Obama says he would create ways for
individuals to buy insurance in groups and would require insurers to sell to
everyone.
That would allow "individuals and small firms to get all the benefits of the
purchasing power of big firms," Obama adviser David Cutler says.
Republican John McCain has made individuals the centerpiece of his health plan.
He proposes $2,500 to $5,000 tax credits to all Americans to purchase their own
coverage and would end the tax breaks workers get for job-based coverage.
McCain says that would even the playing field between those who get coverage at
work and those who buy their own.
Yet even as McCain's advisers advocate expanding the individual market, they
acknowledge the current system is broken.
"The (individual market) right now is not very good," Douglas Holtz-Eakin,
senior policy adviser to McCain, said at a forum in May exploring challenges for
individuals in getting and paying for coverage.
"I don't want to give the impression that the individual or small group market
is a good place to be," Holtz-Eakin said. "It's not. The idea is to create a
better one."
In the current market, insurers selling individual policies try to pick the
healthiest applicants to lower their risks. In most states, insurers can
consider an applicant's health history in deciding whether to offer coverage and
how much to charge.
Insurers "will not cover the sick if they can avoid them," says Len Nichols, an
economist with the New America Foundation, a centrist think tank.
Nichols and other experts say limits on who can get coverage is one of at least
three major problems with the individual market that must be addressed.
The other two are cost and coverage: Is the policy affordable? And will it pay
for what's needed when you get sick?
1. Can you get coverage?
The problem: People who have health problems may be unable to get coverage in
the individual market.
Even if they can, insurers may choose not to cover applicants' "pre-existing"
medical conditions. Excluded conditions vary by insurer.
In a 2001 study by Karen Pollitz of the Georgetown Health Policy Institute,
researchers submitted applications to 19 insurers on behalf of seven fictitious
applicants, who had medical conditions ranging from HIV to allergies. Of 420
applications, 37% were rejected.
"What we have shown is there are carriers who will turn you down if you have hay
fever," Pollitz says.
Insurers say the market isn't all that tough.
A December report by America's Health Insurance Plans, the industry's lobbying
group, examined nearly 1.9 million individual applications. About 18.5% were
withdrawn before the insurer reviewed the person's medical history.
Of the rest, nearly 89% got coverage, although that varied widely by age: About
10% of those ages 30-39 were denied, compared with 29% of those ages 60-64.
Federal law requires insurers to sell policies to certain people who lose group
coverage — including those laid off from their jobs — but sets no limits on what
an insurer can charge.
State efforts and the candidates' solutions: Five states — Maine, Massachusetts,
New Jersey, New York and Vermont — require insurers to sell individual policies
to everyone, regardless of their health. Washington state requires insurers to
take individuals with some health problems.
In May, Iowa Gov. Chet Culver signed a law that requires insurers to cover
pre-existing conditions in new individual applicants — if they previously had
insurance for those conditions and did not let it lapse.
America's Health Insurance Plans says requiring insurers to cover everyone would
raise costs, but its members would agree to offer policies to more applicants in
less-than-perfect health if states would cover those with the most expensive
conditions.
McCain would not require insurers to sell to people with health conditions.
He says he would work with the states to provide some way for people who are
rejected by insurers to get coverage, likely through a state-run program.
Obama would require insurers to sell policies to all applicants.
2. Can you afford it?
The problem: Health insurance costs on the individual market vary widely,
depending on age, health and benefits selected. Generally, younger, healthier
people pay less than older and sicker ones.
The industry's lobbying group says a survey of 2006-07 data from its members
found that premiums paid for coverage ranged from an average of $1,163 a year
for children under 18 to $5,090 a year for people over 60.
By comparison, the average yearly cost to employers for single coverage last
year was $4,479, and workers paid an average of $694 toward that, says a survey
of workplaces by the Kaiser Family Foundation, a non-partisan group that studies
health policy.
Family coverage averaged $12,106 for employers, and workers paid $3,281. Those
plans tend to include more benefits than individual plans.
State efforts and the candidates' solutions: Eighteen states set some limits on
how much can be charged to individuals, often allowing prices to vary based on
age, gender or geographic location, according to the Kaiser foundation.
Two, New York and New Jersey, basically require insurers to charge everyone the
same price. Merrill Matthews of the free-market advocacy group Council for
Affordable Health Insurance says such restrictions raise costs for younger,
healthier people.
A Washington state law took effect in June reinstating the insurance
commissioner's ability to regulate rates. Florida's governor signed a law in May
allowing insurers to sell lower cost "no-frills" insurance with sharply limited
benefits, such as no coverage for specialists.
Obama says allowing individuals to pool together to buy coverage would help
drive the cost down.
He would not allow insurers to charge more based on a person's health, a move
critics such as Matthews say could raise costs for the healthy.
McCain says his plan would help lower prices by allowing people to shop in any
state for health insurance.
Critics such as Georgetown's Pollitz say healthier people would flock to
insurers in the least-regulated states, which could raise rates in other states
that end up covering lots of sick people.
3. What if you get sick?
The problem: Most states allow insurers to cancel policies after patients rack
up large medical bills if insurers find out the applicant purposefully — or, in
some states, even accidentally — left out medical details in the applications.
Insurers say the ability to revoke policies is needed to protect them against
fraud.
State efforts and the candidates' solutions: In California, regulators over the
past year have lodged fines of more than $12 million against several insurers
and ordered three — Blue Cross of California, Kaiser Permanente and Blue Shield
of California — to reinstate people they had dropped, saying they had failed to
show the applicants did anything wrong. Lawsuits from policyholders and the city
of Los Angeles are pending.
In Connecticut, a law took effect in October requiring approval from the state
insurance commissioner before an insurer cancels a policy.
The insurers' lobbying group wants states to pass laws requiring independent
third-party review of policy cancellations after the policies have been
canceled.
Neither presidential candidate has specified his proposal for dealing with
policy cancellations.
Everyone in family insured
The Swaims didn't want to wait for the new president, Congress and the states to
fix the individual market. For them, the solution came when William gave up his
business and took a job with an electrical company that offers health coverage.
Since early May, the entire family has had insurance — with one of the insurers
that had previously rejected Logan, now 8 years old and 44¾ inches tall.
"It would be nice if we could buy our own insurance," says Swaim, a substitute
teacher in Resaca, Ga. "But the problem is that no one can touch insurers. They
can say whether they insure you or not."
Individual health
policies leave many behind, UT, 16.7.2008,
http://www.usatoday.com/news/health/2008-07-16-healthcoverage_N.htm
Psychiatric Group Faces Scrutiny Over Drug Industry Ties
July 12, 2008
The New York Times
By BENEDICT CAREY and GARDINER HARRIS
It seemed an ideal marriage, a scientific partnership that would attack
mental illness from all sides. Psychiatrists would bring to the union their
expertise and clinical experience, drug makers would provide their products and
the money to run rigorous studies, and patients would get better medications,
faster.
But now the profession itself is under attack in Congress, accused of allowing
this relationship to become too cozy. After a series of stinging investigations
of individual doctors’ arrangements with drug makers, Senator Charles E.
Grassley, Republican of Iowa, is demanding that the American Psychiatric
Association, the field’s premier professional organization, give an accounting
of its financing.
The association is the voice of establishment psychiatry, publishing the field’s
major journals and its standard diagnostic manual.
“I have come to understand that money from the pharmaceutical industry can shape
the practices of nonprofit organizations that purport to be independent in their
viewpoints and actions,” Mr. Grassley said Thursday in a letter to the
association.
In 2006, the latest year for which numbers are available, the drug industry
accounted for about 30 percent of the association’s $62.5 million in financing.
About half of that money went to drug advertisements in psychiatric journals and
exhibits at the annual meeting, and the other half to sponsor fellowships,
conferences and industry symposiums at the annual meeting.
This weekend in Chicago, the psychiatry association’s board will meet behind
closed doors, in part to discuss how to respond to the increasingly intense
scrutiny and questions about conflicts of interest.
“With every new revelation, our credibility with patients has been damaged, and
we have to protect that first and foremost,” said Dr. Steven S. Sharfstein, a
former president of the association and now president of the Sheppard Pratt
Health System in Baltimore. “I think we need to review all arrangements between
doctors and industry and be very clear about what constitutes a conflict of
interest and what does not.”
One of the doctors named by Mr. Grassley is the association’s president-elect,
Dr. Alan F. Schatzberg of Stanford, whose $4.8 million stock holdings in a drug
development company raised the senator’s concern. In a telephone interview, Dr.
Schatzberg said he had fully complied with Stanford’s rigorous disclosure
policies and federal guidelines that pertained to his research.
Blocking or constraining researchers from trying to bring medications to market
“will mean less opportunities to help patients with severe illnesses,” Dr.
Schatzberg said, adding, “Drugs that are helpful may not be developed by big
pharmaceutical companies, for a variety of reasons, and we need some degree of
communication between academia and industry” to expand options for patients.
Commercial arrangements are rampant throughout medicine. In the past two
decades, drug and device makers have paid tens of thousands of doctors and
researchers of all specialties. Worried that this money could taint doctors’
research plans or clinical judgment, government agencies, medical journals and
universities have been forced to look more closely at deal details.
In psychiatry, Mr. Grassley has found an orchard of low-hanging fruit. As a
group, psychiatrists earn less in base salary than any other specialists,
according to a nationwide survey by the Medical Group Management Association. In
2007, median compensation for psychiatrists was $198,653, less than half of the
$464,420 earned by diagnostic radiologists and barely more than the $190,547
earned by doctors practicing internal medicine.
But many psychiatrists supplement this income with consulting arrangements with
drug makers, traveling the country to give dinner talks about drugs to other
doctors for fees generally ranging from $750 to $3,500 per event, for instance.
While data on industry consulting arrangements are sparse, state officials in
Vermont reported that in the 2007 fiscal year, drug makers gave more money to
psychiatrists than to doctors in any other specialty. Eleven psychiatrists in
the state received an average of $56,944 each. Data from Minnesota, among the
few other states to collect such information, show a similar trend.
In both states, individual psychiatrists are not top earners, but consulting
arrangements are so common that their total tops all others. The worry is that
this money may subtly alter psychiatrists’ choices of which drugs to prescribe.
An analysis of Minnesota data by The New York Times last year found that on
average, psychiatrists who received at least $5,000 from makers of
newer-generation antipsychotic drugs appear to have written three times as many
prescriptions to children for the drugs as psychiatrists who received less money
or none. The drugs are not approved for most uses in children, who appear to be
especially susceptible to the side effects, including rapid weight gain.
Senator Grassley’s investigations have not only detailed how lucrative those
arrangements can be but have also shown that some top psychiatrists failed to
report all their earnings as required.
After The Times reported on such an arrangement involving Dr. Melissa P.
DelBello of the University of Cincinnati, Mr. Grassley asked the university to
provide her income disclosure forms and asked AstraZeneca, the maker of the
antipsychotic Seroquel, to reveal how much it paid her.
In scientific publications, Dr. DelBello has reported working for eight drug
makers and told university officials that from 2005 to 2007 she earned about
$100,000 in outside income, according to Mr. Grassley.
But AstraZeneca told Mr. Grassley it paid her more than $238,000 in that period.
AstraZeneca sent some of its payments through MSZ Associates, an Ohio
corporation Dr. DelBello established for “personal financial purposes.”
The University of Cincinnati agreed to monitor those payments more closely.
In early June, the senator reported to Congress that Dr. Joseph Biederman, a
renowned child psychiatrist at Harvard Medical School, and a colleague, Dr.
Timothy E. Wilens, had reported to university officials earning several hundred
thousand dollars apiece in consulting fees from drug makers from 2000 to 2007
when in fact they had earned at least $1.6 million each.
Another member of the Harvard group, Dr. Thomas Spencer, reported earning at
least $1 million after being pressed by Mr. Grassley’s investigators. The
Harvard psychiatrists said they took conflict-of-interest policies seriously and
had abided by disclosure rules.
In late June, after Mr. Grassley singled out Dr. Schatzberg, Stanford disputed
some of the numbers in the report and has denied that Dr. Schatzberg violated
any research rules devised to police such conflicts.
In an interview on Wednesday, Dr. Nada L. Stotland, president of the psychiatric
association, said the group had studied Mr. Grassley’s letter and Stanford’s
response and agreed with Stanford. Dr. Schatzberg will take over as president of
the association as planned, she said.
“The larger issue here is that there’s a revolution going on” in how medicine
handles industry money, said Dr. Stotland, a psychiatrist at Rush Medical
College in Chicago. “That’s good, that’s what we need, and I believe we’ve been
on the cutting edge of that revolution in many ways.”
Dr. Stotland said that the association began reviewing the income it received
from pharmaceutical companies last March, to identify potential conflicts.
Doctors and academic researchers generally worked at arm’s length from industry
until the early 1980s, when Congress passed the Bayh-Dole Act. This legislation
encouraged closer collaboration between researchers and industry to bring
products to market more quickly. The act helped foster the growth of the biotech
industry, and soon professors and universities were busy obtaining patents and
building relationships with industry.
Some psychiatrists have long argued that consulting with a company — to help
design a rigorous drug trial, for instance — benefits patients, as long as the
researcher has no financial stake in the product and is not paid to speak about
the drug to other doctors, like a traveling pitchman.
Others say industry and academic researchers are now so deeply intertwined that
exposing doctors’ private arrangements only stokes suspicion without correcting
the real problem: bias.
“Having everyone stand up like a Boy Scout and make a pledge isn’t going to
quell suspicion,” said Dr. Donald Klein, an emeritus professor at Columbia, who
has consulted with drug makers himself. “The only hope to rule out bias is to
have open access to all data that’s produced in studies and know that there are
people checking it” who are not on that company’s payroll.
Studies have shown that researchers who are paid by a company are more likely to
report positive findings when evaluating that company’s drugs. The private deals
can directly affect patient care, said Dr. William Niederhut, a psychiatrist in
private practice in Denver who receives no industry money.
Dr. Niederhut said company-sponsored doctors had spread the word that new and
expensive drugs were better in treating bipolar disorder than lithium, the
cheaper old standby treatment.
“It’s a sales pitch, and now it’s looking like a whole lot of people would have
done better if they’d started on lithium in the first place,” Dr. Niederhut said
in a telephone interview. “The profession absolutely has to come clean on these
industry deals, and soon.”
Tighter rules, stronger statements and more debate may not make much difference,
if Mr. Grassley’s findings are any guide. Universities have rules requiring that
faculty members disclose their outside income so that conflicts of interest in
research or patient care can be managed. But some of the psychiatrists named in
the investigations apparently ignored the rules.
“I think we may be coming to a point where hospitals and medical schools have to
get serious about sanctioning,” said Dr. Paul S. Appelbaum, director of the
division of psychiatry, medicine and the law at Columbia. “You can suspend
doctors’ privileges, or suspend their right to treat patients; both have a huge
impact on income and career. But if you’re serious about these disclosure
policies, you have to be willing to back them up.”
Psychiatric Group Faces
Scrutiny Over Drug Industry Ties, NYT, 12.7.2008,
http://www.nytimes.com/2008/07/12/washington/12psych.html?em&ex=1216094400&en=6972653468dc83ca&ei=5087%0A
Dr. Michael DeBakey Is Dead at 99
July 12, 2008
By THE ASSOCIATED PRESS
Filed at 2:57 a.m. ET
The New York Times
HOUSTON (AP) -- Dr. Michael DeBakey, the world-famous cardiovascular surgeon
who pioneered such now-common procedures as bypass surgery and invented a host
of devices to help heart patients, died Friday night at The Methodist Hospital
in Houston, officials announced. He was 99.
DeBakey died from ''natural causes,'' according to a written statement issued
early Saturday by spokesmen for Baylor College of Medicine and The Methodist
Hospital.
DeBakey surgery in February 2006 for a damaged aorta -- a procedure he had
developed.
DeBakey counted world leaders among his patients and helped turn Baylor College
of Medicine in Houston from a provincial school into one of the nation's great
medical institutions.
''Dr. DeBakey's reputation brought many people into this institution, and he
treated them all: heads of state, entertainers, businessmen and presidents, as
well as people with no titles and no means,'' said Ron Girotto, president of The
Methodist Hospital System.
Girotto said the surgeon ''has improved the human condition and touched the
lives of generations to come.''
While still in medical school in 1932, he invented the roller pump, which became
the major component of the heart-lung machine, beginning the era of open-heart
surgery. The machine takes over the function of the heart and lungs during
surgery.
It was only a start of a lifetime of innovation. The surgical procedures that
DeBakey developed once were the wonders of the medical world. Today, they are
commonplace procedures in most hospitals.
He also was a pioneer in the effort to develop artificial hearts and heart pumps
to assist patients waiting for transplants, and helped create more than 70
surgical instruments.
Dr. Michael DeBakey Is
Dead at 99, NYT, 12.7.2008,
http://www.nytimes.com/aponline/us/AP-Obit-DeBakey.html?hp
Age of Riches
Challenges of $600-a-Session Patients
July 7, 2008
The New York Times
By ERIC KONIGSBERG
Not long ago, a young titan of New York real estate sat in his
psychotherapist’s office. An art collector, he was thinking of bidding about $8
million for a painting, and something about the deal made him uneasy.
The therapist thought the patient was merely trying to impress him. This
happened whenever the man felt unsure of himself, which was most of the time.
But instead of trying to explore the patient’s anxiety, the therapist encouraged
him to buy the artwork: “This is what you want; you should go get it.”
T. Byram Karasu, a Manhattan psychiatrist whom the therapist consulted about the
patient, was appalled. “That was precisely the wrong treatment,” he said. “The
doctor forgot that addiction cannot be satisfied by its object. The therapist’s
job is not to comfort and validate the patient’s excesses and consumption. Those
are neuroses.”
Dr. Karasu, known as an expert in treating the wealthy and powerful, recognized
a common pitfall among his peers: Rich people can be seductive. “The therapist
wants to identify with the patients and comes to see it as his role to help them
get more wealthy,” he said. In the process, the doctor risks becoming the
patient’s “alter-id.”
Wealth reminiscent of the Gilded Age has encouraged a thriving business for a
small and highly specialized group of therapists in New York and elsewhere.
Their daily work gives them an intimate view of an elite who differ in some ways
from their predecessors, and who can test the therapists who treat them.
More than a dozen therapists who are respected by their peers in the counseling
of extremely wealthy patients said in interviews that, as with the real estate
mogul, it can be hard to resist the temptation to sycophantically adopt their
point of view.
In some cases, the patients treat their therapists as but another member of
their entourage of servants. Some therapists also cited a heightened difficulty
with frustration and setbacks for people used to getting what they wanted. And
they are resistant to opening up, to showing vulnerability.
Dr. Karasu said the past few years had felt different to him.
“The problems are the same, but the scale is different now,” he said. “Hedge
funds — there is no product, only wealth. It is flabbergasting to my patients,
too. They can make so much money at once and then lose it.”
Dr. Michael H. Stone, a psychiatrist affiliated with Columbia, said that the
preponderance of patients with self-made fortunes, many made at a relatively
young age, marked a striking shift.
“It used to be that my patients were the children of the rich: inheritors,
people who suffered from the neglect of jet-setting parents or from the fear
that no matter what they did, they would never measure up to their father’s
accomplishments,” he recalled. “Now I see so many young people — people in their
30s and 40s — who’ve made the money themselves.”
Dr. Stone said those two kinds of patients tended to have different problems:
“In my experience, there was a high incidence of depression in the people who
were born rich. And by contrast, the people today who are making a fortune are
so often narcissistic in a way that excludes depression.”
Dr. Karasu is chairman of the department of psychiatry and behavioral sciences
at Albert Einstein College of Medicine in the Bronx. He also has an office for
private practice on 88th Street near Fifth Avenue. He charges $600 for a
45-minute session, seeing most of his patients at least twice a week.
It was during his first week in practice, in 1969, that he inherited a famous
patient from a psychoanalyst who had recently passed away, and from that point
on, he said: “My patients trained me in these issues. There’s a real school for
it.”
King Ludwig Syndrome
A couple of years ago, Dr. Karasu received a call on behalf of an entertainment
executive who wanted to reschedule an appointment at the last minute.
Dr. Karasu said the only time he had available that week was at 7 one night. The
executive’s assistant said: “He’s having dinner then. How about 10 p.m.? He’s
flying out to the Hamptons, but we’ll send a car for you and you can ride with
him and do therapy on the helicopter, and then we’ll send you home in the
morning.”
On and on it went. “If I would say I am busy on Saturday, the assistant would
offer to pay me extra, as if that would be the answer,” Dr. Karasu said, adding
that he declined the request. “For the average patient, the 45 minutes with a
therapist is the most precious time. For this patient, it was just another
activity superimposed on his schedule, and the therapist has to accommodate his
way of being — like his trainer, his cook, his pilot, his administrative staff.”
Dr. Karasu and several of his peers voiced a concern that a rich person today
was ever more inclined to view his or her psychotherapist as nothing more than a
highly skilled member of his personal army.
Most of his patients have been “mega-successes, in very public industries,” he
said. A good many work in the highest reaches of the financial sector, and some
have been “celebrities in the movie business.” He also travels to Washington
every Tuesday to counsel a couple of patients with high-profile jobs in
politics. (“We’re not talking about congressmen,” he said.)
Dr. Karasu, 73, is a slight and measured fellow who, much like the patients he
describes, possesses an immediately apparent curiosity and ambition. He grew up
in a prosperous Jewish household in Istanbul, where his father was a
newspaperman and wrote thrillers. Dr. Karasu has written several books,
including an autobiographical novel, a forthcoming collection of poetry, and
“The Art of Marriage Maintenance,” co-written with his wife, Sylvia, who is also
a psychiatrist.
Dr. Karasu acknowledged that he was not immune from taking satisfaction in the
success and fame of his patients. “Wealthy people bring about a degree of awe,
even in their therapists sometimes,” he said. “This is the biggest problem I see
in the doctors I supervise. And these are fully practicing doctors, doctors
making $400, $500 an hour.”
He added: “It’s King Ludwig Syndrome. In the 19th century, Bernhard von Gudden
was the psychiatrist for the Bavarian royal family and began to treat King
Ludwig II, who was psychotic. In the end, the two of them drowned in a boat. So
I teach my people who are treating wealthy people, ‘Don’t get in your patients’
boats.’ ”
Wealthy patients find Dr. Karasu — and others of his ilk — as they would other
providers of goods and service: through word of mouth and through a general
insistence on being referred to therapists with high academic credentials. For
example, friends of Stephen A. Schwarzman, chief executive of the Blackstone
Group, say that he has referred them to Dr. Karasu. A Blackstone spokesman said,
“Mr. Schwarzman does not comment on personal conversations.”
It is the extremely rare member of this circle who does not acknowledge
struggling with complicated and contradictory feelings about superrich patients.
The therapists admitted to feeling jealous or contemptuous on occasion, and
though Dr. Karasu said of his patients, “They are, almost all of them, smarter
than I am, and certainly more competent,” he rarely missed an opportunity in
interviews for a joke or aside about the absurdity of talking about wealth as an
affliction.
Janet L. Wolfe, a Park Avenue psychologist and the co-author of a paper about
difficulties in counseling “women of the ‘upper’ classes,” said she considered a
rich person’s unhappiness or emotional anguish no less serious than anybody
else’s, but acknowledged how trivial some of her patients’ problems could sound.
“One of the things that drew a very wealthy woman to see me was that she was an
inadequate tennis player,” Dr. Wolfe recalled. “She was very serious about this.
She felt that the other wealthy women she played with would think she was an
inadequate person. It’s easier for rich patients to take problems like this
seriously.”
Slow to Trust
The politician would not listen to his therapist.
In fact, nobody — not the Harvard-educated foreign policy specialist who was
supposed to be advising him, and certainly not Dr. Karasu — could persuade him
that he was wrong. About anything.
It was anxiety that had brought the man to therapy , and both the cause and the
symptoms followed a pattern. “He had learned how to maneuver everyone to come
around to his point of view,” Dr. Karasu said. “He had removed the foreign
policy consultant from his circle after the man had disagreed with him.”
Dr. Karasu saw this as an opportunity to press the patient. “But this person
knows more than you,” he told the elected official, a wealthy businessman who
had turned to public service, yearning for a greater challenge, after quickly
making a fortune in the private sector.
“But I’m his boss,” the patient insisted.
“The issue wasn’t foreign affairs; it was control,” Dr. Karasu recalled. “That
was his attitude to me as well: ‘I know what is best because look at who I am.’
”
While it is common for a patient to resist treatment, Dr. Karasu said, “There
are some people who, no matter how intelligent they are, they think they know my
business better than I do. And they are very difficult to reach.”
Most of the therapists interviewed said the rich were also far more able than
the average patient to not show up for a session or give up on therapy
altogether. “It starts with the way it’s so easy for them to not show up for an
appointment because it means nothing to them if they’re out the $300 or $400,”
said Dr. Stone, who is also known as a forensic psychiatrist and is the host of
a show on the Investigation Discovery network.
Part of the therapeutic model for many practitioners involves charging whether
the patient shows up or not: The idea of obligation — and the notion that there
be some cost incurred for not meeting it — becomes essential to the treatment.
“Superbly well-to-do people tend to have much less of an impetus to work through
things now,” Dr. Stone said. “They have so many opportunities to seek
gratification that they’re not hurting in the same way. I’m thinking of a
narcissistic and unmarried patient in his late 40s who, in another time and
under most circumstances, you’d have said missed the boat. He could get
gratification through his wealth and move from one model to another, so that he
didn’t really need to maintain a relationship.”
That patient, Dr. Stone said, terminated therapy abruptly by way of a call —
from his secretary — informing him that the man had left for Africa on a
spontaneous vacation.
Moreover, the environments in which a lot of these patients have become
successful do not necessarily leave them well equipped to benefit from the
talking cure. “To generalize, it’s not the priority of people who are successful
on Wall Street to be intimate,” Dr. Karasu said. “It is their priority to be
aggressive. Many will not open themselves up to intimacy even in love affairs.
They are slow to trust anyone — even the therapist.”
One patient with whom he had been making progress, Dr. Karasu said, walled
himself off from him ever more after a business accomplishment made him famous
and pushed his considerable wealth to stratospheric levels. “I said, ‘What is
happening to you that you are regressing now, when you are thriving?’ ” Dr.
Karasu recounted. “He said, ‘The higher up the monkey goes,’ ” the easier it was
for the public to catch a glimpse of his posterior. “He was terrified that the
world was out to make a fool of him,” Dr. Karasu added.
Great Disenchantments
It is not uncommon to find in wealthy and powerful patients an extremely low
tolerance for frustration, the therapists said.
Dr. Seth Aidinoff, a NewYork-Presbyterian Hospital psychiatrist who practices on
the Upper East Side and also consults for hedge funds and Wall Street firms,
illustrated the consequences with the Saturday-afternoon choice faced by “your
typical master of the universe,” who can either play outside with his 7-year-old
or stay inside to complete a business deal on the phone.
“The phone call might involve the most important and interesting people in the
world, being well compensated for his time, and the chance to handle it with
A-plus skill,” Dr. Aidinoff said. “Whereas playing with his 7-year-old might be
sort of boring, or unsatisfying; his son might not fully express his
appreciation, or the child could even be in a bad mood. So this person might
find himself terrified of spending time with his child because it’s not an
activity he can control or succeed at the high level of accomplishment to which
he is accustomed.”
Because so much of ordinary life is built on small failures and frustrations,
therapists see among this patient group a great disenchantment. The therapists
cited familiar tropes of the new gilded age: the three-year renovation of a
country house that becomes its own “infrastructure of entrapment,” as one
therapist put it; the man so accustomed to travel by private jet and chauffeur
that he develops a fear of airports and taxis. “It results in a fear of chaos
and vulnerability” Dr. Aidinoff said.
“These people have to win,” Dr. Karasu said. He described another patient, a
tennis enthusiast, who was so humiliated when his 16-year-old son began beating
him that he gave up playing.
“He said: ‘It’s a silly game. You just hit the ball, they hit it back. What is
to be gained from this?’ ” Dr. Karasu said. “After that, he tried to discourage
his son from playing.”
A patient’s inability to accept his own limitations is not without beneficial
side effects, he said. “I see this in the way my patients are consumed by the
idea of their deaths, or their attempts to counteract death,” Dr. Karasu said.
“All of the philanthropy you see — the buildings named after people for giving
$50 million to this museum or to Columbia — is a result of one man after another
trying to conquer his mortality.”
Challenges of
$600-a-Session Patients, NYT, 7.7.2008,
http://www.nytimes.com/2008/07/07/nyregion/07therapists.html?hp
Costly Cancer Drug Offers Hope, but Also a Dilemma
July 6, 2008
The New York Times
By GINA KOLATA and ANDREW POLLACK
It took only an instant for 58-year-old Gailanne Reeh to go from the picture
of health to death’s door. By chance, her doctor noticed a lump under her arm
during a routine exam. It turned out to be advanced breast cancer.
Soon she was having tests to reveal the extent of the cancer and hearing the
grim results.
The surgeon, she recalled, “looked at me and said: ‘This is not a conversation I
like to have. But I can’t do anything for you. You can’t be cured. You can’t be
treated. All we can do is manage your cancer.’ ” On scans to detect tumors, the
doctor told Ms. Reeh, “you light up like a Christmas tree.”
And so, like many others in that situation, Ms. Reeh, the vivacious owner of a
staffing agency in Boston, was given bevacizumab, also known as Avastin, a drug
that signifies both the hopes and dilemmas of modern medicine.
Looked at one way, Avastin, made by Genentech, is a wonder drug. Approved for
patients with advanced lung, colon or breast cancer, it cuts off tumors’ blood
supply, an idea that has tantalized science for decades. And despite its price,
which can reach $100,000 a year, Avastin has become one of the most popular
cancer drugs in the world, with sales last year of about $3.5 billion, $2.3
billion of that in the United States.
But there is another side to Avastin. Studies show the drug prolongs life by
only a few months, if that. And some newer studies suggest the drug might be
less effective against cancer than the Food and Drug Administration had
understood when the agency approved its uses.
While many patients and their doctors say the drug can improve the quality of
life — like a sense of well-being and an ability to carry out daily tasks
without exhaustion or pain — such effects can be hard to document. Meanwhile,
many patients with cancers other than those of the colon, lung or breast are
taking the drug, even in cases where there is no compelling evidence that it can
help.
Avastin also has serious, if infrequent, side effects, some of which can be
lethal. And because it is almost always used with standard chemotherapy — it did
not work as well when researchers tried it alone — patients on Avastin do not
escape chemotherapy’s side effects.
“I still use Avastin routinely, but it’s sobering,” Dr. Leonard Saltz, a colon
cancer specialist at Memorial Sloan-Kettering Cancer Center in New York, said of
the new data. “It’s not a slam dunk and, in fact, the incremental benefit may be
more modest than we want to admit.”
If Avastin were inexpensive or if it cured cancer or even held it at bay, as the
drug Gleevec does for blood cancer, few might care. But like a half-dozen or so
new biotechnology drugs with a similar combination — alluring promise, high
price and only arguable benefits — Avastin raises troubling questions:
What does it mean to say an expensive drug works? Is slowing the growth of
tumors enough if life is not significantly prolonged or improved? How much
evidence must there be before billions of dollars are spent on a drug? Who
decides? When, if ever, should cost come into the equation?
For a patient like Ms. Reeh, fighting for her life, the cost is not the main
concern. If her insurer did not pay, she said, she would go into debt, find a
way to raise the money.
But some in the pharmaceutical industry worry that such prices will raise
concerns about whether the drugs are worth it, leading to a backlash like price
controls or restrictions on use.
Roy Vagelos, a former chief executive of Merck who is considered an elder
statesman of the industry, said in a recent speech that he was troubled by a
drug, which he would not name but which was a clear reference to Avastin, that
costs $50,000 a year and adds four months of life. “There is a shocking
disparity between value and price,” he said, “and it’s not sustainable.”
Some patient advocates are also troubled by very expensive treatments like
Avastin coming into routine use on what they see as little more than a hope and
an expensive prayer.
“It’s absolutely critical that we start having a public discussion,” said
Barbara Brenner, executive director of Breast Cancer Action, an advocacy group.
“I think of Avastin as a model that is showing us where the problem is.”
The Rising Cost
The problem is largely one of cost.
Cancer drugs constitute the second biggest category of drugs in the United
States behind cholesterol-lowering medicines, and accounted for $17.8 billion of
total prescription drug sales of $286.5 billion in 2007, according to IMS
Health, a health care information company. Spending on drugs for cancer grew 14
percent last year, faster than for all but three other diseases.
About 100,000 Americans take Avastin, according to Genentech’s data. The drug is
being formally tested in as many as 450 clinical trials for about 30 types of
cancer. And Genentech, its partner Roche and the National Cancer Institute are
now starting studies that will include more than 26,000 people with lung, colon
or breast cancer at earlier stages of the disease than were studied initially.
If Avastin is approved for those earlier-stage patient groups, it could have a
major impact in delaying the return of their cancer, but hundreds of thousands
of additional people could end up taking it, possibly for years.
And that, insurers and patient advocates say, could impose a considerable
financial burden.
The drug’s price, as charged by Genentech, can be $4,000 to more than $9,000 a
month, depending on a patient’s weight and the type of cancer. Avastin’s cost to
patients and insurers can be much higher, though, because doctors and hospitals
buy the drug and then sell it to patients or their insurers, often marking up
the price. So the $2.3 billion that Genentech recorded in sales of Avastin
represents only part of what Americans spent on the drug last year.
And while doctors typically want the best for their patients, there also are
other factors that may push them to prescribe Avastin.
“Think about where the interests are aligned,” said Dr. Deborah Schrag, a colon
cancer specialist at the Dana-Farber Cancer Institute in Boston. “Patients who
seek out cancer care are often quite willing to try all kinds of things. Doctors
want to help them and may be financially incentivized. And it is often quite
hard for insurance companies to intervene.”
Medicare requires that the doctor or hospital buying Avastin be paid an amount
equal to Genentech’s average selling price plus a markup of 5 to 6 percent. Of
that amount, Medicare pays 80 percent and the patient pays 20 percent. Doctors
and hospitals typically do not make much money on Avastin for Medicare patients,
and can even lose money if they buy the drug at a price that is higher than
average. But patients can end up paying thousands of dollars a month. Some have
supplemental insurance to take care of it; others do not.
But private insurers sometimes pay several times as much as Medicare pays for
Avastin. Doctors and hospitals have at times charged as much as $35,000 a month
for the drug, said Dr. Peter Dumich, who reviews claims for cancer patients for
AWAC, a company that helps employers contain health care costs. The insurers
have little choice, Dr. Dumich says, when their contracts say they must pay a
portion, like 80 percent of the charge, whatever the charge actually is.
“Providers have them over a barrel,” he said.
And, like Medicare, private insurers may in turn require patients to pay a
percentage of what can be hefty bills.
That has happened to Jim Lemieux, a colon cancer patient at Dana-Farber. His
private insurance requires that he pay 25 percent of the cost of his treatment,
which includes Avastin. His insurer, he said, is charged $6,000 a month for the
drug, making his share $1,500.
Mr. Lemieux, who was a sales manager at a car dealership, says he cannot bear to
look at his medical bills. They include bills for hospitalizations and surgery
and co-payments for standard chemotherapy, as well as Avastin.
To try to make ends meet, he and his wife just sold their house and are moving
into their son’s basement. Even so, he says, he expects he will have to file for
bankruptcy.
“You figure you’ve got insurance,” Mr. Lemieux said. “I paid 30 years and never
got sick. I should have just paid the money to myself.”
But he is not planning to give up Avastin.
“I’m trying to stay alive,” Mr. Lemieux said. “I decided I’m not going to die
from Stage 4 colon cancer.”
A Promising Dream
When Napoleone Ferrara was hired by Genentech in 1988, he was assigned to work
on a drug to ease labor during childbirth. But he could not get cow pituitary
glands out of his mind.
Dr. Ferrara had noticed in his previous academic job that when he mixed extracts
from the glands with cells from blood vessels, the vessel cells started to grow
rapidly. Something made by those glands, he reasoned, could spur vessel growth.
He found that substance in 1989 and called it vascular endothelial growth
factor, or VEGF (pronounced VEJ-eff). He even isolated its gene. And that led to
a new idea for a cancer drug.
It drew from a hypothesis for a sort of universal cancer treatment, advanced by
the late Dr. Judah Folkman of Harvard. Dr. Folkman had argued, starting in 1971,
that tumors must grow their own blood vessels to bring them nourishment and
oxygen. If you could choke off those vessels, Dr. Folkman said, you could halt
cancers.
Dr. Ferrara and his colleagues realized that if they could block VEGF, cancer
cells might not be able to grow blood vessels. So Genentech developed a
monoclonal antibody, a type of protein, that would bind to VEGF and disable it.
In 1997, the company began testing its antibody, which became Avastin, in cancer
patients.
There were some setbacks. Avastin failed in its first big clinical trial,
against very advanced breast cancer. Genentech’s stock dropped 10 percent in one
day, and some analysts questioned whether the company’s investment would ever
pay off.
Meanwhile, the company was well into a trial of Avastin for colorectal cancer.
Patients got chemotherapy plus either Avastin or a placebo. The Avastin patients
lived more than four months longer, a median of 20.3 months, compared with 15.6
months for the other group. “We were excited,” Dr. Schrag said. “Four months is
big.”
In February 2004, 15 years after Dr. Ferrara’s initial discovery, the Food and
Drug Administration approved Avastin for patients with advanced colon cancer. A
blockbuster was born.
But now there is a question mark over that evidence. That first exciting result
compared Avastin with a type of chemotherapy that has since been widely replaced
by a more effective regimen.
In a later, larger study comparing Avastin with current chemotherapy, Avastin
slowed the growth of tumors but did not extend life by an amount considered
statistically significant.
Dr. Schrag said she would continue to give the drug to her colon cancer
patients. But when she talks to patients about Avastin now, she said, she will
add a few more caveats.
She believes that some patients are helped — that they may feel better and, she
hopes, may even, in some cases, live longer. She says a few of her Avastin
patients lived several years and some are still alive. Of course, she
acknowledges, there is no proof that Avastin was responsible, but it is stories
like those that give her, and patients, hope.
“All patients want to be the tail end of the survival curve,” Dr. Schrag said.
When Avastin was approved for colon cancer, Genentech decided to charge $2,200
for an average dose, taken every two weeks. That was a reflection of the
research and development it had put into the drug as well as continuing
research, said Walter Moore, the company’s director of government relations.
Genentech, which has never before revealed what it spent to develop Avastin, now
says that it and its partner Roche have spent more than $2.25 billion starting
with Dr. Ferrara’s original work. The figure includes research, clinical trials
and filing for regulatory approval and is well beyond what was spent by the
federal government, which conducted important clinical trials of Avastin.
Through May 2006, the government had spent $44.6 million on Avastin trials and
related laboratory work, according to figures obtained from the National Cancer
Institute by Consumer Watchdog, an advocacy group.
While it is impossible to compare directly the company’s investment to the costs
of developing other cancer drugs, the amount Genentech says it spent is “on the
high side” of the industry average, said Henry Grabowski, a professor of
economics at Duke University who has analyzed drug development costs.
Genentech says it and Roche — which owns a majority of Genentech and markets
Avastin outside the United States — will spend an additional $1 billion testing
Avastin as a treatment for early-stage cancers.
The price also reflected Genentech’s perceived value of the drug compared with
other cancer treatments. The price was half that of Erbitux, a colon cancer drug
from ImClone Systems and Bristol-Myers Squibb that was approved the same month
as Avastin and had not been shown to prolong life.
But Avastin is typically used for a longer time and by more patients than
Erbitux. And the Avastin dose for lung and breast cancer is twice that for colon
cancer, doubling the price.
Eric Schmidt, an analyst at Cowen and Company, said pharmaceutical companies
typically based drug prices on what the market could bear.
“It’s high because Genentech can price it high,” he said, noting that Avastin’s
price was in line with that of some other cancer drugs. Despite the company’s
research and development costs, Mr. Schmidt said, Genentech is one of the most
profitable of pharmaceutical and biotechnology companies.
Other countries have different views about whether Avastin is worth its price.
An institute that advises the British government on which drugs to pay for
recommended against it, saying that the drug was not cost effective based on its
cost per year of life extended.
In the United States, Genentech argues that it puts patients first, with free
drugs for those who have no way to pay for them and donations to charities that
can help with payments. It also capped the price for a year’s supply of Avastin
at $55,000 (not counting markups by doctors and hospitals) for patients with
incomes of less than $100,000 a year.
But progress against cancer has a price, the company says.
“The quest is to eliminate the disease,” Arthur D. Levinson, Genentech’s chief
executive, said at an annual investor meeting. “And, yes, there is going to be a
cost to that.”
Of Dubious Benefit
After colon cancer, the next target was lung cancer.
Dr. Bruce Johnson of Dana-Farber knew the difficulties well. He had been at the
National Cancer Institute, where he reviewed 25 years’ worth of clinical trials,
30 studies that started with high hopes and ended with little progress. He used
to give talks quoting a World War I general: “Ground gain minimal. Casualties
huge. Conclusion — press on.”
Avastin, in that context, looked like something of a triumph. Patients who took
it along with standard chemotherapy survived for a median of 12.3 months,
compared with 10.3 months for those getting only chemotherapy. The results were
announced in 2005. “Finally,” Dr. Johnson said, “something worked.”
But as with colon cancer, a newer study adding Avastin to a different
chemotherapy regimen has raised questions about its effectiveness against lung
cancer. The study’s Avastin patients lived no longer than those who got the
chemotherapy plus placebo. Although the drug did slow the median time until
progression of tumors, the difference was less than a month.
The third approval for Avastin, for advanced breast cancer, came in February of
this year. The clinical trial found it significantly slowed the progression of
cancer but did not significantly extend life. The F.D.A. went against its own
panel of outside experts, who had voted 5 to 4 against approval.
The agency’s action has not sat well. Senator Charles E. Grassley, Republican of
Iowa, asked the Government Accountability Office to look into the F.D.A.’s
approval of Avastin and some other drugs that “appear to have little to no
effect in protecting lives and increasing health.”
Dr. Lee Newcomer, an oncologist and executive at the insurer United HealthCare,
said patients were not well served, and neither were insurers, nor the public,
which ultimately foots the bill. If a drug just stops tumor progression, without
the woman’s living longer or feeling better, without her noticing anything
different, Dr. Newcomer said, “you’re treating an X-ray.”
Patient advocacy groups were split.
“Even when these drugs ‘work,’ what kind of impact are you talking about?” said
Fran Visco, president of the National Breast Cancer Coalition, which opposed
approval. “But we market them and give them to everybody.”
Yet other doctors and advocates for patients say that when tumors grow, patients
can notice new or worsening symptoms. And they certainly experience greater
anxiety.
Dr. Kathy Albain, a breast cancer specialist at Loyola University Medical Center
in Maywood, Ill., polled colleagues and patients and found overwhelming support
for approving drugs based on delaying tumor progression. It would be ideal to
show that a drug also prolongs life, but that may not be realistic, she said.
The reason is that when a woman’s cancer progresses, doctors change the drugs
they use, hoping to slow the cancer. That dilutes any impact of the first drug —
in this case Avastin.
Kay Wissmann, director for government relations at the Breast Cancer Network of
Strength, a patient advocacy group, said women should have a choice to use
Avastin.
“We’ve got some good evidence about this particular drug,” she said, “so maybe
we should let the people with metastatic disease have the option of using it.”
Unapproved Uses
Then there are patients who cannot wait for evidence that a drug works for their
cancer.
One patient’s husband had no medical training. But he determined through his own
literature search that his wife’s form of brain cancer produced a lot of VEGF,
the very substance Avastin neutralized. So the couple wanted to try Avastin,
even though it had never been tested for brain cancer. It was 2004, when the
only Avastin approval was for colon cancer.
They asked the woman’s doctor, Dr. Virginia Stark-Vance, to give them the drug.
Dr. Stark-Vance, a solo practitioner in Dallas and Fort Worth, was reluctant,
worried that Avastin could cause bleeding in the brain. That had happened in one
of the earliest clinical trials, when a 29-year-old woman whose liver cancer had
spread to her brain collapsed from a hemorrhage while riding her bicycle.
Finally, Dr. Stark-Vance agreed on the condition that the woman be hospitalized
to receive Avastin, in case there was a brain hemorrhage. Had there been one,
Dr. Stark-Vance “could have lost her license,” said Dr. Henry Friedman, a brain
cancer specialist at Duke.
Like many others taking Avastin, this woman plunged into the unknown, without
the assurance of a clinical trial studying whether the drug worked for her type
of cancer.
Doctors are free to prescribe Avastin, or any other drug on the market, for
unapproved uses, at their discretion. As much as 75 percent of cancer drug use
is of this “off label” variety, according to an estimate by the National
Comprehensive Cancer Network, a group of big cancer centers. And some doctors
say that with patients dying, they simply cannot wait for airtight evidence.
“Of course we want everything to be evidence-based,” said Dr. Yashar Hirshaut,
an oncologist in Manhattan. “I also like the American flag and apple pie.”
But, he explained, “You say, ‘This person is dying right here and I need
something that will help, and there’s a logical construct that I can see how it
will help.’ ”
One of his patients, Alice Lichter, has had gastric cancer since 2006. Dr.
Hirshaut is throwing the whole arsenal at it, giving her gemcitabine, a drug
used for pancreatic cancer, plus virtually every drug approved for colon cancer:
Avastin, Erbitux, Eloxatin, irinotecan, 5-FU and leucovorin. Most are not
approved for gastric cancer.
Once every two to four weeks, Ms. Lichter, 72, flies from her home in Miami and
checks into Lenox Hill Hospital in Manhattan, where she undergoes four days of
intravenous infusions.
“I call Lenox Hill my second home,” she said.
‘You Name It, It Got Tried’
Ms. Lichter, whose cancer appears to have receded, said she never questioned Dr.
Hirshaut’s judgment. And she has no idea how much her drugs cost because
Medicare is paying for them and her supplemental insurance covers her
co-payment. Insurers say they are often forced by state laws to pay for cancer
drugs not approved by the Food and Drug Administration, and Medicare must pay if
the drug’s use is listed in a compendium, a reference compiled by cancer
specialists, whose standards are looser than the F.D.A.’s.
Such requirements are one reason about 12 percent of United HealthCare’s Avastin
patients have cancers other than colon, breast and lung. “Brain, stomach,
pancreas, primary cancers of the liver, bladder, small bowel, larynx, prostate —
you name it, it got tried,” Dr. Newcomer said.
But the anecdotes and evidence from small trials that may seem to justify
off-label use sometimes turn out to be misleading. That happened with pancreatic
cancer. After patients and doctors decided Avastin had to be helping, cancer
researchers themselves conducted a large study. So did Roche. Avastin, both
studies concluded, did not prolong life for people with cancer of the pancreas.
For brain cancer, doctors are encouraged, although they do not really know for
sure whether Avastin helps. The brain tumor in Dr. Stark-Vance’s patient shrank
so much after two infusions of Avastin that the radiologist who performed the
brain scans called Dr. Stark-Vance in wonderment.
Dr. Stark-Vance began treating more patients. Some insurers paid for the drug.
Others, including Medicare and Medicaid, did not. But Dr. Stark-Vance said
Genentech agreed to provide the drug free for her patients who could not
otherwise pay.
As word spread, Dr. Friedman at Duke and Genentech organized studies of a type
generally considered less than definitive. There was no control group that took
another drug or got a placebo. Everyone got Avastin. Otherwise, no one would
enroll in the study, doctors argued.
Then the investigators compared the results with what they thought would have
happened without Avastin. The patients lived a median of about nine months,
about three months longer than the researchers estimate would have been
expected.
But such comparisons have led scientists seriously astray in the past because
the people being treated with a new drug often are very different from previous
patients who did not take it and because overall medical care steadily improves.
Nonetheless, Genentech has said it planned to apply this year to the F.D.A. for
approval for Avastin to treat glioblastoma, the deadliest form of brain cancer.
Dr. Stark-Vance said her initial Avastin brain cancer patient broke her hip and
had to be taken off the drug because it interfered with wound healing. She
eventually died.
But by now, even without an F.D.A. approval, “the whole country” is using
Avastin for glioblastoma, Dr. Friedman said.
Better Than Nothing?
Gailanne Reeh remembers what life was like within a few months of those initial
scans, when her cancer began causing terrible symptoms.
Her abdomen grew so full of fluid that it was hard to bend to tie her shoes.
Bowel movements were difficult, and even lying down was uncomfortable with that
huge mass in her abdomen.
She says she was chilled by what she recalls her doctor saying: “There was so
much growing so fast in my abdomen and so much in my bowel, it was not a matter
of maybe I would get a bowel obstruction. It was when I would get a bowel
obstruction,” Ms. Reeh said. “And when I got it, there would be nothing anyone
could do. I would die.”
To try to stave off such a horrible outcome, her oncologist, Dr. Eric Winer of
Dana-Farber, offered to enroll her in a clinical trial comparing Avastin with
another new biotech drug. Ms. Reeh was assigned to the group that got Avastin in
combination with the chemotherapy drug paclitaxel, also known as Taxol.
The study closed after six months, but Ms. Reeh continued with her drug regimen,
and her insurer is paying. After six months of treatment the fluid in her
abdomen was down to just a trace, her tumors were stable or smaller and she felt
like her former self again.
“I’m really, really excited,” she said.
Was it the Avastin?
Dr. Winer said he did not know, since Taxol can also shrink tumors. It is
impossible to draw conclusions from individual patients, he said. Still, he
said, “I think it is quite likely that the combination of Taxol and Avastin
improved her odds of having a better quality of life.”
Dr. Winer says that when he is not sitting in front of a patient, he thinks
about whether drugs like Avastin are worth it to society. But when facing a
seriously ill patient, who, based on clinical trial results, might benefit —
even if only a little — from Avastin along with chemotherapy, he has to think
about his patient’s needs.
“I can’t say, ‘Let’s not use Avastin; it’s a very expensive drug and I am
worried about the cost to society,’ ” Dr. Winer said.
And so, Dr. Winer said, the answer you get when you ask whether drugs like
Avastin are worth it very much depends on whom you ask.
“A person who hasn’t been affected by cancer will say, ‘Gee, why should we pay
for an expensive treatment that doesn’t extend life when we have other needs?’ ”
Dr. Winer said.
A person like Ms. Reeh will have a different response. She does not want to give
up Avastin.
Last month, she reluctantly stopped taking her drugs for a while because Taxol
was injuring the nerves in her feet. But later this month she hopes to resume
taking both drugs, or at least Avastin.
Ms. Reeh says she knows her cancer may very well kill her eventually. But what
is it worth to feel better again?
“It’s really about living and not waiting to die,” she said.
And what if 5 percent of Avastin patients live a lot longer than they would have
without the drug?
“I might be in that 5 percent,” she said.
Costly Cancer Drug
Offers Hope, but Also a Dilemma, NYT, 6.7.2008,
http://www.nytimes.com/2008/07/06/health/06avastin.html?hp
Push in Bronx for H.I.V. Test for All
June 26, 2008
The New York Times
By ANEMONA HARTOCOLLIS
The New York City health department plans to announce on Thursday an
ambitious three-year effort to give an H.I.V. test to every adult living in the
Bronx, which has a far higher death rate from AIDS than any other borough. The
campaign will begin with a push to make the voluntary testing routine in
emergency rooms and storefront clinics, where city officials say that cumbersome
consent procedures required by state law have deterred doctors from offering the
tests.
“Routine would mean if you came into the emergency room for asthma or a broken
leg, we test everyone for H.I.V., if they’re willing,” the health commissioner,
Dr. Thomas R. Frieden, said in an interview on Wednesday.
While Manhattan has long been the epicenter of the AIDS epidemic in New York,
with the highest incidence of both AIDS and H.I.V., the virus that causes it,
the Bronx, with its poorer population, has far more deaths from the disease.
Public health officials attribute this to people not getting tested until it is
too late to treat the virus effectively, thus turning a disease that can now be
managed with medication into a death sentence.
Several AIDS experts said on Wednesday that the Bronx campaign was the most
aggressive testing effort they could recall in the nation. Two years ago,
Washington, D.C., made a high-profile push to test 450,000 residents, enlisting
celebrity endorsements and distributing 80,000 free testing kits, but the
campaign resulted in only about 45,000 people being tested.
“What’s new here is that we are implementing it on this large a level,” said Dr.
Donna Futterman, director of the adolescent AIDS program at Montefiore Medical
Center in the Bronx, who helped New York develop the new program. “The Bronx has
1.3 million people. It’s bigger than most cities, bigger than Boston, bigger
than Washington. We’re talking about a significant urban population.”
City officials estimate that 40 percent of the 830,000 people ages 18 to 64 in
the Bronx have been tested for H.I.V. in the past year. Half of the remainder,
about 250,000 people, have never been tested, and the goal is to test them
first. Tests would be given at 40 designated sites, including clinics, community
centers, churches and emergency rooms. Dr. Monica Sweeney, an assistant health
commissioner for H.I.V. prevention, said the city had not set aside money
specifically for the program, but would absorb the $12 cost of each test.
In organizing the campaign, which formally begins on Friday, Dr. Frieden has
enlisted support from elected officials, health care providers and clergy
members in the Bronx. But the proposal is raising some concerns.
Outside the Neighborhood and Family Health Center on East 149th Street in the
South Bronx, Melissa Sierra, 20, expressed concern on Wednesday that the focus
on the Bronx would reinforce “a lot of stereotypes” about the borough. “It might
keep people away,” she said.
Dr. Frieden said the health department had chosen the borough because it had
good relationships with clinics and hospitals there. “I think we are thinking of
it, and the Bronx will think of it, as the Bronx being first to know, a
community taking the lead in responding,” he said.
Robert E. Bank, chief operating officer of Gay Men’s Health Crisis, and Earl
Brown, the deputy borough president in the Bronx, both said on Wednesday that
they hoped the program would be extended citywide.
“Brooklyn is a horribly devastated borough,” Mr. Bank said. “Manhattan is a
highly impacted borough, Queens is a highly impacted borough.”
Indeed, the rate of AIDS cases is highest in Manhattan, at 82 per 100,000
people, compared with 75 in the Bronx, 46 in Brooklyn, 26 in Queens and 16 on
Staten Island, according to state health statistics compiled last year. But the
rate of deaths from AIDS is highest in the Bronx, at 37 per 100,000 residents,
compared with 21 for Manhattan, 19 for Brooklyn, 8 for Staten Island and 6 for
Queens.
City officials said that Bronx residents are already more likely to be tested
than adults in other boroughs (they estimate that 28 percent of Manhattanites,
24 percent of adults in Queens, 29 percent in Brooklyn and 17 percent on Staten
Island have been tested in the last year).
The campaign to make testing routine, as Dr. Frieden put it, comes after years
of lobbying by him and others to overhaul strict state regulations, which have
changed little since the dawn of the AIDS epidemic in the 1980s, when H.I.V.
testing was perceived more as a public-health tracking system than as a
diagnostic tool. The regulations require patients to give written permission for
testing after being counseled on the process, which many doctors found onerous
and time-consuming.
Dr. Frieden said New York’s consent law is among the nation’s most rigid. The
federal Centers for Disease Control and Prevention recommends routine H.I.V.
testing with doctors simply informing patients that the test will be given
unless they decline.
San Francisco County Hospital, Dr. Frieden said, saw an increase of 17 percent
in testing and 36 percent in positive results within three months of switching
from written to oral consent in 2006.
Dr. Futterman, who is also a professor of clinical pediatrics at Albert Einstein
College of Medicine, said she hoped that changing the mentality surrounding
H.I.V. testing to make it a routine part of a patient’s blood work — along with,
say, cholesterol tests — would galvanize state legislators to ease its consent
rules.
“Everything in AIDS has changed except the old testing paradigm,” Dr. Futterman
said. “Old school was that you had to tell them everything that could happen.
That starts to seem cruel. If you go for cancer diagnosis, they don’t make the
doctor say what you’re going to do if your mammogram is positive.”
The written consent requirement, she said, has been a barrier in emergency
rooms, where doctors often feel it interferes with more immediate needs.
Under the new initiative, hospital administrators in the Bronx have agreed to
test in emergency rooms, while still following state consent law. Dr. Futterman
said she had carefully constructed a script for doctors that follows state law
but squeezes what is typically a 20-minute counseling and consent process into
five minutes. A doctor with lots of experience could deliver the script in three
minutes, she said, and her own record is one minute.
Using that streamlined process, Dr. Futterman said, she had increased the
proportion of her patients being tested to 20 or 25 percent, from 10 percent.
Dr. Frieden said that city clinics for sexually transmitted diseases had testing
rates as high as 60 percent, and the city jail at Rikers Island tested nearly 30
percent.
Mr. Bank said Gay Men’s Health Crisis opposes eliminating written consent, but
would relax the process so that patients are given a form with two boxes, one
saying they want to be tested, the other saying they do not.
In an effort to make H.I.V. testing less intimidating, the city will issue
public service announcements and information on the 311 hot line. It is also
posting tear-off sheets with addresses of testing centers in places like
check-cashing stores, where residents can discreetly slip them into pockets.
“It’s not about one group doing it, it’s about everybody doing it,” said Dr.
Sweeney of the health department. Community organizations, universities,
churches and politicians, she said, “are going to have all their constituents
that come to them for other services, they’re going to use it as an opportunity
to say, ‘Get your H.I.V. test.’ ”
Dmitry Kiper contributed reporting.
Push in Bronx for H.I.V.
Test for All, NYT, 26.6.2008,
http://www.nytimes.com/2008/06/26/nyregion/26hiv.html
Expert says worms and parasites drain U.S. poor
Tue Jun 24, 2008
2:24pm EDT
Reuters
By Maggie Fox, Health and Science Editor
WASHINGTON (Reuters) - Diseases caused by worms and parasites are draining
the health and energy of the poorest Americans, an expert said on Tuesday.
And diseases associated with the developing world, such as dengue fever and
Chagas disease, may become a bigger problem for the United States as the climate
changes, said Dr. Peter Hotez of George Washington University and the Sabin
Vaccine Institute in Washington.
"The message is a little tough because they are not killer diseases -- they
impact on child development, intellectual development, hearing and sometimes
even heart disease," Hotez said in a telephone interview.
He said the diseases help to keep people mired in poverty, as infections may
last years, decades or even lifetimes.
"Throughout the American South during the early twentieth century, malaria
combined with hookworm infection and pellagra (a vitamin deficiency) to produce
a generation of anemic, weak, and unproductive children and adults," Hotez
wrote.
The parasitic diseases are having similar effects now, he said.
Hotez reviewed nine diseases affecting at least 10 million Americans for a
report in the journal Public Library of Science Neglected Tropical Diseases,
which he also edits.
"These diseases occur predominantly in people of color living in the Mississippi
Delta and elsewhere in the American South, in disadvantaged urban areas, and in
the U.S.-Mexico borderlands, as well as in certain immigrant populations and
disadvantaged white populations living in Appalachia," he wrote.
They include ascariasis, the most common human worm infection. It is caused by a
parasitic worm that lives in the intestine, and infected just under 4 million
people in 1974 according to the last survey, in the South and Appalachia.
DOG DROPPINGS
Toxocariasis, a roundworm parasite transmitted in dog droppings, infected up 2.8
million poor black children living in inner cities, the South and Appalachia,
Hotez said. The U.S. Centers for Disease Control and Prevention estimates these
roundworms, which can cause intestinal illness and blindness, infect up to 14
percent of the U.S. population.
Strongyloidiasis is caused by a threadworm that lives throughout the body and
infects 68,000 to 100,000 people. It may cause a hyper-immune reaction in some
people.
Cysticercosis caused by the pork tapeworm and giardiasis, a diarrheal illness
caused by a one-celled parasite, are also common, Hotez said.
One threat to babies is cytomegalovirus, which infects 27,002 newborn annually,
causing deafness and mental retardation.
"It's amazing what we tolerate," Hotez said. He noted the United States spends
$1 billion a year preparing for outbreaks of diseases that have not occurred,
including smallpox, anthrax and avian influenza.
"But these (other) diseases are occurring among voiceless people," he said.
"It's an unintended form of racism in a sense. We need to make these disease
household words."
Chagas disease, caused by the parasite Trypanosoma cruzi, infects as many as 8
to 11 million people in Latin America and may become a U.S. threat, Hotez said.
"In Louisiana, almost 30 percent of the armadillos and 38 percent of the
opossums are infected with T. cruzi, and a case of Chagas disease was recently
reported in post-Katrina New Orleans," he wrote.
"In the coming decade, global warming and increased flooding in the region could
combine to promote dengue and Chagas disease epidemics among the poor in
Louisiana."
Dengue, carried by mosquitoes, can sometimes cause a deadly hemorrhagic fever
and has been reported in Texas.
(Reporting by Maggie Fox; Editing by Julie Steenhuysen and Doina Chiacu)
Expert says worms and
parasites drain U.S. poor, R, 24.6.2008,
http://www.reuters.com/article/newsOne/idUSN2435994920080624
Bill with billions in health plan cuts passes House
Tue Jun 24, 2008
1:11pm EDT
Reuters
WASHINGTON (Reuters) - The U.S. House of Representatives on Tuesday approved
a bill that would shave billions of dollars in reimbursement from health plans
that contract with the federal Medicare program.
Payment would be cut to health insurers such as Aetna Inc and Humana Inc under
the bill sponsored by Democrats Charles Rangel of New York and John Dingell of
Michigan.
U.S. lawmakers face a June 30 deadline to pass legislation blocking a scheduled
11 percent pay cut for Medicare doctors. Cuts to the private plans would help
keep the doctors' payments intact.
In the Senate, Republicans and Democrats are working on a compromise that could
be announced as early as Tuesday afternoon. Other Medicare providers that are
likely to be affected include oxygen companies such as Apria Healthcare and
wheelchair makers like Invacare Corp.
(Reporting by Kim Dixon; Editing by Lisa Von Ahn)
Bill with billions in
health plan cuts passes House, R, 24.6.2008,
http://www.reuters.com/article/newsOne/idUSWBT00926020080624
Doctors Say Medication Is Overused in Dementia
June 24,
2008
The New York Times
By LAURIE TARKAN
Ramona
Lamascola thought she was losing her 88-year-old mother to dementia. Instead,
she was losing her to overmedication.
Last fall her mother, Theresa Lamascola, of the Bronx, suffering from anxiety
and confusion, was put on the antipsychotic drug Risperdal. When she had trouble
walking, her daughter took her to another doctor — the younger Ms. Lamascola’s
own physician — who found that she had unrecognized hypothyroidism, a disorder
that can contribute to dementia.
Theresa Lamascola was moved to a nursing home to get these problems under
control. But things only got worse. “My mother was screaming and out of it,
drooling on herself and twitching,” said Ms. Lamascola, a pediatric nurse. The
psychiatrist in the nursing home stopped the Risperdal, which can cause
twitching and vocal tics, and prescribed a sedative and two other
antipsychotics.
“I knew the drugs were doing this to her,” her daughter said. “I told him to
stop the medications and stay away from Mom.”
Not until yet another doctor took Mrs. Lamascola off the drugs did she begin to
improve.
The use of antipsychotic drugs to tamp down the agitation, combative behavior
and outbursts of dementia patients has soared, especially in the elderly. Sales
of newer antipsychotics like Risperdal, Seroquel and Zyprexa totaled $13.1
billion in 2007, up from $4 billion in 2000, according to IMS Health, a health
care information company.
Part of this increase can be traced to prescriptions in nursing homes.
Researchers estimate that about a third of all nursing home patients have been
given antipsychotic drugs.
The increases continue despite a drumbeat of bad publicity. A 2006 study of
Alzheimer’s patients found that for most patients, antipsychotics provided no
significant improvement over placebos in treating aggression and delusions.
In 2005, the Food and Drug Administration ordered that the newer drugs carry a
“black box” label warning of an increased risk of death. Last week, the F.D.A.
required a similar warning on the labels of older antipsychotics.
The agency has not approved marketing of these drugs for older people with
dementia, but they are commonly prescribed to these patients “off label.”
Several states are suing the top sellers of antipsychotics on charges of false
and misleading marketing.
Ambre Morley, a spokeswoman for Janssen, the division of Johnson & Johnson that
manufactures Risperdal, would not comment on the suits, but said: “As with any
medication, the prescribing of a medication is up to a physician. We only
promote our products for F.D.A.-approved indications.”
Nevertheless, many doctors say misuse of the drugs is widespread. “These
antipsychotics can be overused and abused,” said Dr. Johnny Matson, a professor
of psychology at Louisiana State University. “And there’s a lot of abuse going
on in a lot of these places.”
Dr. William D. Smucker, a member of the American Medical Directors Association,
a group of health professionals who work in nursing homes, agreed. Though the
group encourages doctors to conduct a thorough assessment and prescribe
antipsychotics only as a last resort, he said, “Many physicians are absent
without leave in the nursing home and don’t take an active role in the
assessment of the patient.”
Some nursing homes are trying a different approach, so-called environmental
intervention. The strategies include reducing boredom, providing intellectual
and physical stimulation, exercise, calming music, bringing in pets for therapy
and improving how the staff approaches and talks to dementia patients.
At the Margaret Teitz Nursing and Rehabilitation Center in Queens, social
workers do life reviews of patients to understand their interests, lifestyle and
former occupations.
“I had a patient who used to be in fashion,” said Nancy Goldwasser, the director
of social services. “So we got her fabric samples. And she’d sit and look
through the books, touch the fabric, and it would calm her.”
But such approaches are time consuming, they do not help all patients, they can
be prohibitively expensive and they will be more difficult to provide as
Alzheimer’s continues to increase.
“Our health care system isn’t set up to address the mental, emotional and
behavioral problems of the elderly,” said Dr. Gary S. Moak, president of the
American Association for Geriatric Psychiatry.
Nursing homes are short staffed, and insurers do not generally pay for the
attentive medical care and hands-on psychosocial therapy that advocates
recommend. It is much easier to use sedatives and antipsychotics, despite their
side effects.
The first generation of antipsychotics, like Haldol, carry a significant risk of
repetitive movement disorders and sedation. Second-generation antipsychotics,
also called atypicals, are more commonly prescribed because the risk of movement
disorders is lower. But they, too, can cause sedation, and they contribute to
weight gain and diabetes.
Used correctly, the drugs do have a role in treating some seriously demented
patients, who may be incapacitated by paranoia or are self-destructive or
violent. Taking the edge off the behavior can keep them safe and living at home,
rather than in a nursing home.
If patients are prescribed an antipsychotic, it should be a very low dose for
the shortest period necessary, said Dr. Dillip V. Jeste, a professor of
psychiatry and neuroscience at the University of California, San Diego.
It may take a few weeks or months to control behavior. In many cases, the
patient can then be weaned off of the drugs or kept at a very low dose.
Some experts say another group of medications — antidementia drugs like Aricept,
Exelon and Namenda — are underused. Research shows that 10 to 20 percent of
Alzheimer’s patients had noticeable positive responses to the drugs, and 40
percent more showed some cognitive improvement, even if it was not noticeable to
an observer.
“Sometimes, it’s enough to take the edge off the behavioral problems, so the
family and patient can live with it and you don’t expose people to much risk,”
said Dr. Gary J. Kennedy, director of geriatric psychiatry at the Montefiore
Medical Center in the Bronx.
Other experts cite a lack of research backing these drugs for behavioral
problems.
If patients begin showing behavioral symptoms of dementia, doctors said, they
should have complete medical and psychiatric workups first, especially if
symptoms develop suddenly.
“Just because someone is 95 does not mean one should not do a workup, especially
if she’s been healthy,” Dr. Kennedy said.
Common causes of the symptoms include ministrokes, reparable brain hemorrhage
from a mild bump on the head, hypothyroidism, dehydration, malnourishment,
depression and sleep disorders.
Some doctors point out that simply paying attention to a nursing home patient
can ease dementia symptoms. They note that in randomized trials of antipsychotic
drugs for dementia, 30 to 60 percent of patients in the placebo groups improved.
“That’s mind boggling,” Dr. Jeste said. “These severely demented patients are
not responding to the power of suggestion. They’re responding to the attention
they get when they participate in a clinical trial.
“They receive both T.L.C. and good general medical and humane care, which they
did not receive until now. That’s a sad commentary on the way we treat dementia
patients.”
To family members looking at a nursing home for an aging parent, experts
recommend seeking out homes with low staff turnover, a high ratio of staff
members to patients, and programs with psychosocial components.
The Medicare Web site has basic information on individual homes at
www.medicare.gov/NHcompare. The National Citizens’ Coalition for Nursing Home
Reform, at www.nccnhr.org, offers a consumer guide to choosing a nursing home.
If medications are necessary, a family member should communicate with the
prescribing doctor, learn the goal of each medication and be involved in making
the decision.
Dr. Moak, of the psychiatry association, emphasized seeking out the doctor.
Family members, he said, “often speak through the nursing staff, and that’s a
huge mistake.”
Family members who are not convinced that a relative is receiving the best care
should get a second opinion, as Ramona Lamascola did.
The physician she consulted, Dr. Kennedy of Montefiore, stopped her mother’s
antipsychotics and sedatives and prescribed Aricept.
“It’s not clear whether it was getting her hypothyroid and other medical issues
finally under control or getting rid of the offending medications,” he said.
“But she had a miraculous turnaround.”
Theresa Lamascola still has dementia, but she went from confinement in a
wheelchair — unable to sit still and screaming out in fear — to being able to
walk with help, sit peacefully, have some memory and ability to communicate,
understand subtleties of conversations and even make jokes.
Or, as her daughter put it, “I got my mother back.”
Doctors Say Medication Is Overused in Dementia, NYT,
24.6.2008,
http://www.nytimes.com/2008/06/24/health/24deme.html
Second
Opinion
From a
Prominent Death, Some Painful Truths
June 24,
2008
The New York Times
By DENISE GRADY
Apart from
its sadness, Tim Russert’s death this month at 58 was deeply unsettling to many
people who, like him, had been earnestly following their doctors’ advice on
drugs, diet and exercise in hopes of avoiding a heart attack.
Mr. Russert, the moderator of “Meet the Press” on NBC News, took blood pressure
and cholesterol pills and aspirin, rode an exercise bike, had yearly stress
tests and other exams and was dutifully trying to lose weight. But he died of a
heart attack anyway.
An article in The New York Times last week about his medical care led to e-mail
from dozens of readers insisting that something must have been missed, that if
only he had been given this test or that, his doctors would have realized how
sick he was and prescribed more medicine or recommended bypass surgery.
Clearly, there was sorrow for Mr. Russert’s passing, but also nervous
indignation. Many people are in the same boat he was in, struggling with weight,
blood pressure and other risk factors — 16 million Americans have coronary
artery disease — and his death threatened the collective sense of well-being.
People are not supposed to die this way anymore, especially not smart,
well-educated professionals under the care of doctors.
Mr. Russert’s fate underlines some painful truths. A doctor’s care is not a
protective bubble, and cardiology is not the exact science that many people wish
it to be. A person’s risk of a heart attack can only be estimated, and although
drugs, diet and exercise may lower that risk, they cannot eliminate it entirely.
True, the death rate from heart disease has declined, but it is still the
leading cause of death in the United States, killing 650,000 people a year.
About 300,000 die suddenly, and about half, like Mr. Russert, have no symptoms.
Cardiologists say that although they can identify people who have heart disease
or risk factors for it, they are not so good at figuring out which are in real
danger of having an attack soon, say in the next year or so. If those patients
could be pinpointed, doctors say, they would feel justified in treating them
aggressively with drugs and, possibly, surgery.
“It’s the real dilemma we have in cardiology today,” said Dr. Sidney Smith, a
professor of medicine at the University of North Carolina and a past president
of the American Heart Association. “Is it possible to identify the group at
higher short-term risk?”
What killed Mr. Russert was a plaque rupture. A fatty, pimplelike lesion in a
coronary artery burst, and a blood clot formed that closed the vessel and cut
off circulation to part of the heart muscle. It was a typical heart attack, or
myocardial infarction, an event that occurs 1.2 million times a year in the
United States, killing 456,000 people.
In Mr. Russert’s case, the heart attack led to a second catastrophe, an abnormal
heart rhythm that caused cardiac arrest and quickly killed him. An electric
shock from a defibrillator might have restarted his heart if it had been given
promptly when he collapsed at his desk. But it was apparently delayed.
Dr. Smith and other cardiologists say the main problem is that there is no way
to figure out who has “vulnerable plaques,” those prone to rupture. Researchers
are trying to find biomarkers, substances in the blood that can show the
presence of these dangerous, ticking time-bomb plaques. So far, no biomarker has
proved very accurate.
Mr. Russert’s heart disease was a mixed picture. Some factors looked favorable.
There was no family history of heart attacks. Though he had high blood pressure,
drugs lowered it pretty well, said his internist, Dr. Michael A. Newman. His
total cholesterol was not high, nor was his LDL, the bad type of cholesterol, or
his C-reactive protein, a measure of inflammation that is thought to contribute
to plaque rupture. He did not smoke. At his last physical, in April, he passed a
stress test, and his heart function was good. Dr. Newman estimated his risk of a
heart attack in the next 10 years at 5 percent, based on a widely used
calculator.
On the negative side, Mr. Russert had low HDL, the protective cholesterol, and
high triglycerides. He was quite overweight; a waist more than 40 inches in men
increases heart risk. A CT scan of his coronary arteries in 1998 gave a calcium
score of 210, indicating artery disease — healthy arteries do not have calcium
deposits — and a moderate to high risk of a heart attack. An echocardiogram in
April found that the main heart pumping chamber had thickened, his ability to
exercise had decreased slightly, and his blood pressure had increased a bit. Dr.
Newman and his cardiologist, Dr. George Bren, changed his blood pressure
medicines, and the pressure lowered to 120/80, Dr. Newman said.
Another blood test, for a substance called apoB, might have been a better
measure of risk than LDL, some doctors say. Others disagree.
Some doctors say people like Mr. Russert, with no symptoms but risk factors like
a thickened heart, should have angiograms, in which a catheter is threaded into
the coronary arteries, dye is injected, and X-rays are taken to look for
blockages. Some advocate less invasive CT angiograms. Both types of angiogram
can identify plaque deposits, and if extensive disease or blockages at critical
points are found, a bypass is usually recommended. But the tests still cannot
tell if plaques are likely to rupture, Dr. Smith and other cardiologists say.
And Mr. Russert’s doctors did not think that an angiogram was needed.
An autopsy found, in addition to the plaque rupture, extensive disease in Mr.
Russert’s coronary arteries, enough to surprise his doctors, they said. Had they
found it before, Dr Newman said, a bypass would have been recommended. Dr. Bren
differed, saying many cardiologists would still not have advised surgery.
Given all the uncertainties, what’s a patient to do?
“You want to be sure your blood pressure and lipids are controlled, that you’re
not smoking, and you have the right waist circumference,” Dr. Smith said.
Statins can reduce the risk of dying from a heart attack by 30 percent, he said.
“But what about the other 70 percent?” Dr. Smith asked. “There are other things
we need to understand. There’s tremendous promise, but miles to go before we
sleep.”
From a Prominent Death, Some Painful Truths, NYT,
24.6.2008,
http://www.nytimes.com/2008/06/24/health/24hear.html
New
estimates show diabetes affects 24 million
Tue Jun 24,
2008
1:22pm EDT
Reuters
WASHINGTON
(Reuters) - New government estimates show that nearly 24 million people in the
United States have diabetes, an increase of more than 3 million in two years.
This means that nearly 8 percent of the U.S. population has diabetes, mostly the
type-2 diabetes linked with obesity, poor diet and a lack of exercise, the U.S.
Centers for Disease Control and Prevention said on Tuesday.
The estimates, based on 2007 data, also show that 57 million people have
pre-diabetes, a condition that puts people at increased risk for diabetes. And
up to 25 percent of people with diabetes do not know they have it, the CDC said
-- down from 30 percent two years ago.
Almost 25 percent of the population 60 years and older had diabetes in 2007, the
CDC found.
The highest rates are among Native Americans and Alaska Natives, with 16.5
percent affected.
Close to 12 percent of blacks and 10 percent of Hispanics have diabetes, but
just 7.5 percent of Asian Americans and 6.6 percent of whites.
Diabetes causes the body to produce less insulin, or to use it less effectively,
which in turn causes blood sugar levels to rise. This in turn damages blood
vessels and organs, leading to blindness, kidney disease, limb loss and heart
disease.
It is the seventh-leading cause of death in the United States.
"It is concerning to know that we have more people developing diabetes, and
these data are a reminder of the importance of increasing awareness of this
condition, especially among people who are at high risk," said Dr. Ann Albright,
director of the CDC's Division of Diabetes Translation.
"On the other hand, it is good to see that more people are aware that they have
diabetes. That is an indication that our efforts to increase awareness are
working, and more importantly, that more people are better prepared to manage
this disease and its complications."
(Reporting
by Maggie Fox; Editing by Julie Steenhuysen)
New estimates show diabetes affects 24 million, R,
24.6.2008,
http://www.reuters.com/article/domesticNews/idUSN2435588720080624
Bernanke
Says Health Costs a Strain
June 17,
2008
The New York Times
By THE ASSOCIATED PRESS
WASHINGTON
— Bolstering the performance of the health care system is one of the biggest
challenges facing the country, the Federal Reserve chairman, Ben S. Bernanke,
said Monday.
New medical technologies and treatments are allowing people to live healthier,
longer and more productive lives. However, the aging of millions of baby boomers
coupled with rapidly rising heath care costs are accounting for an ever-growing
share of both personal and government budgets — strains that will become
increasingly burdensome unless changes are made, the Fed chief said.
Challenges, he said, fall into three major areas: improving access to health
care for the 47 million Americans — or about 16 percent of the population — who
lack health insurance; bolstering the quality of care; and controlling costs.
“Improving the performance of our health care system is without a doubt one of
the most important challenges our nation faces,” Mr. Bernanke said in remarks on
health care changes organized by a Senate panel on Capitol Hill.
On his remarks, the Fed chief did not talk about the Fed’s next move on interest
rates or the state of the economy.
Many economists believe the Fed will hold a key interest rate steady at 2
percent, a four-year low, when it meets next week. Mr. Bernanke and other Fed
officials have sent strong signals that the Fed’s rate-cutting campaign, started
last September to shore up the ailing economy, was probably over because of
mounting concerns about inflation.
Wall Street investors and some other believe that the Fed might be forced to
raise rates later this year to thwart a dangerous inflation flare-up. Others,
however, still think the Fed will be able to hold rate steady through the rest
of this year.
It is a difficult spot for Fed policy makers. They are trying to aid an economy
that has been badly bruised by the blows of a housing, credit and financial
debacles. At the same time, they don’t want inflation to take off. If the Fed
were to start boosting rates too soon to fend off inflation, that could deal a
set back to already fragile economic growth.
On the health care front, Mr. Bernanke did not recommend specific solutions,
saying the difficult choices involved with improving access and quality and
controlling costs were best left to policy makers in Congress, the White House
and elsewhere.
“Taking on these challenges will be daunting,” he said. Given the complexity of
health care matters, he suggested that it might be better for policymakers to
consider an “eclectic approach,” rather than one single set of changes to
address all concerns.
“We may need to first address the problems that seem more easily managed rather
than waiting for a solution that will address all problems at once,” Mr.
Bernanke offered.
Bernanke Says Health Costs a Strain, NYT, 17.6.2008,
http://www.nytimes.com/2008/06/17/business/17fed.html?hp
Plan
Seeks More Access for Disabled
June 16,
2008
The New York Times
By ROBERT PEAR
WASHINGTON
— The Bush administration is about to propose far-reaching new rules that would
give people with disabilities greater access to tens of thousands of courtrooms,
swimming pools, golf courses, stadiums, theaters, hotels and retail stores.
The proposal would substantially update and rewrite federal standards for
enforcement of the Americans With Disabilities Act, a landmark civil rights law
passed with strong bipartisan support in 1990. The new rules would set more
stringent requirements in many areas and address some issues for the first time,
in an effort to meet the needs of an aging population and growing numbers of
disabled war veterans.
More than seven million businesses and all state and local government agencies
would be affected. The proposal includes some exemptions for parts of existing
buildings, but any new construction or renovations would have to comply.
The new standards would affect everything from the location of light switches to
the height of retail service counters, to the use of monkeys as “service
animals” for people with disabilities, which would be forbidden.
The White House approved the proposal in May after a five-month review. It is
scheduled to be published in the Federal Register on Tuesday, with 60 days for
public comment. After considering those comments, the government would issue
final rules with the force of law.
Already, the proposal is stirring concern. The United States Chamber of Commerce
says it would be onerous and costly, while advocates for disabled Americans say
it does not go far enough.
Since the disability law was signed by the first President Bush, advances in
technology have made services more available to people with disabilities. But
Justice Department officials said they were still receiving large numbers of
complaints. In recent months, the federal government has settled lawsuits
securing more seats for disabled fans at Madison Square Garden in New York and
at the nation’s largest college football stadium, at the University of Michigan.
The Census Bureau says more than 51 million Americans have some kind of
disability, with nearly two-thirds of them reporting severe impairments.
The proposed rules, under development for more than four years, flesh out the
meaning of the 1990 law, which set forth broad objectives. The 215,000-word
proposal includes these new requirements:
¶Courts would have to provide a lift or a ramp to ensure that people in
wheelchairs could get into the witness stand, which is usually elevated from
floor level.
¶Auditoriums would have to provide a lift or a ramp so wheelchair users could
“participate fully and equally in graduation exercises and other events” at
which members of the audience have direct access to the stage.
¶Any sports stadium with a seating capacity of 25,000 or more would have to
provide safety and emergency information by posting written messages on
scoreboards and video monitors. This would alert people who are deaf or hard of
hearing.
¶Theaters must provide specified numbers of seats for wheelchair users (at least
five in a 300-seat facility). Viewing angles to the screen or stage must be
“equivalent to or better than the average viewing angles provided to all other
spectators.”
¶Light switches in a hotel room could not be more than 48 inches high. The
current maximum is 54 inches.
¶Hotels must allow people with disabilities to reserve accessible guest rooms,
and they must honor these reservations to the same degree they guarantee other
room reservations.
¶At least 25 percent of the railings at fishing piers would have to be no more
than 34 inches high, so that a person in a wheelchair could fish over the
railing.
¶At least half of the holes on miniature golf courses must be accessible to
people using wheelchairs, and these holes must be connected by a continuous,
unobstructed path.
¶A new swimming pool with a perimeter of more than 300 feet would have to
provide “at least two accessible means of entry,” like a gentle sloping ramp or
a chair lift.
¶New playgrounds would have to provide access to slides, swings and other play
equipment for children who use wheelchairs.
The Justice Department acknowledged that some of the changes would have
significant costs. But over all, it said, the value of the public benefits,
estimated at $54 billion, exceeds the expected costs of $23 billion.
In an economic analysis of the proposed rules, the Justice Department said the
need for an accessible environment was greater than ever because the Iraq war
was “creating a new generation of young men and women with disabilities.”
John L. Wodatch, chief of the disability rights section of the Justice
Department, said: “Disability is inherent in the human condition. The vast
majority of individuals who are fortunate enough to reach an advanced age will
benefit from the proposed requirements.”
By 2010, the department estimates, 2 percent of the adult population will use
wheelchairs, and 4 percent will use crutches, canes, walkers or other mobility
devices. Likewise, it said, as the population ages, the number of people with
hearing loss will increase.
Under the 1990 law, businesses are supposed to remove barriers to people with
disabilities if the changes are “readily achievable,” meaning they can be
“carried out without much difficulty or expense.”
The Bush administration is proposing a safe harbor for small businesses. They
could meet their obligations in a given year if, in the prior year, they had
spent at least 1 percent of their gross revenues to remove barriers.
Curtis L. Decker, executive director of the National Disability Rights Network,
a coalition of legal advocates, said: “Safe harbors make us very nervous. A
small business could spend the requisite amount of money and still not be
accessible.”
Randel K. Johnson, a vice president of the United States Chamber of Commerce,
said the proposed rules “are so long and technically complex that even the
best-intentioned small business could be found out of compliance by a clever
lawyer looking to force a settlement.”
The Justice Department cited the “monetary cost cap” as one of several steps it
was taking to limit the rules’ impact on small businesses. But Mr. Johnson said
he feared that courts would view the ceiling as a floor and tell businesses they
should spend 1 percent of their revenues on removing barriers.
The proposed rules affirm the right of people with disabilities to use guide
dogs and other service animals in public places, but they tighten the definition
to exclude certain species.
When the existing rules were adopted in the early 1990s, the Justice Department
said, few people anticipated the current trend toward “the use of wild, exotic
or unusual species” as service animals.
The proposed rules define a service animal as “any dog or other common domestic
animal individually trained to do work or perform tasks” for a person with a
physical or mental disability.
Under this definition, the administration says, monkeys could not qualify as
service animals, nor would reptiles; amphibians; rabbits, ferrets and rodents;
or most farm animals.
Under the rules, a hotel, restaurant, theater, store or public park could ask a
person with a disability to remove a service animal if the animal was out of
control or not housebroken, or if it posed a direct threat to the health or
safety of others.
By way of example, the rules say that a theater could exclude a dog that
disrupted a live performance by repeated barking.
The rules confirm that people with disabilities can use traditional wheelchairs,
power wheelchairs and electric scooters in any public areas open to pedestrians.
But shopping centers, amusement parks and other public places could impose
reasonable restrictions on two-wheeled Segway vehicles, golf carts and “other
power-driven mobility devices” used by those with disabilities.
Plan Seeks More Access for Disabled, NYT, 16.6.2008,
http://www.nytimes.com/2008/06/16/washington/16disabled.html
Editorial
The
Massachusetts Model
June 16,
2008
The New York Times
Massachusetts’s pioneering plan to provide universal health coverage is off to a
good start and is heartening evidence that national health care reform may be
possible if sufficient skill and determination are applied to forge a political
consensus.
The state requires that all residents take out health insurance or suffer tax
penalties if they don’t. It also requires employers to offer coverage to their
workers or make alternative payments if they don’t. As it enters what could be a
critical year in determining its viability, the plan can claim some substantial
successes.
It has already covered some 350,000 of the uninsured — more than half of the
roughly 650,000 residents who were estimated to be uninsured when the plan began
in 2006. Two-thirds of the new enrollees signed up for subsidized coverage
available to low-income people. The rest signed up for private commercial
insurance, either through their employers, or on their own, or through a new
“connector” organization that funnels people to unsubsidized private plans.
Critics — opponents of new entitlement programs are watching closely — are
accurate when they say that coverage is hardly universal if 300,000 people still
don’t have insurance. But the plan is in its early days. Enrollment has grown
faster than expected, especially for a complex, newly established program.
The real test will come this year, when higher penalties for those who fail to
get coverage will kick in and we will see whether coverage can really be made
mandatory without sparking political resistance. So far, polls show increasing
public support.
Massachusetts has also held premium increases in the unsubsidized component of
the program to 5 percent, far less than the previous double-digit increases. It
has reformed the costly individual insurance market so that everyone can now get
insurance at low group rates — an opportunity unavailable elsewhere.
Two of the original concerns — that people might drop private insurance to gain
subsidized coverage or that businesses might dump employees on the state program
— have not materialized. On the downside, many of the newly insured reported
difficulty finding a primary care physician, and the share of low-income
residents using emergency rooms for nonemergency care rose slightly, the
opposite of what was supposed to happen.
The chief criticism, however, is that costs have risen faster than the original
projections, forcing the state to raise its spending estimates for the current
fiscal year from $472 million to $625 million and from $725 million to $869
million for next year. The shortfall occurred mostly because the state
underestimated the number of uninsured residents and how fast low-income people
would sign up for subsidized coverage. It is a warning to other states to keep
projections realistic.
The key challenge will be to keep costs under control and find new sources of
revenue while maintaining widespread support for the program. How well
Massachusetts handles that challenge will determine whether its pioneering
health plan falls into a financial pit or points the way toward universal
coverage.
The Massachusetts Model, NYT, 16.6.2008,
http://www.nytimes.com/2008/06/16/opinion/16mon1.html
Letters
Doctors,
Research and Drug Payments
June 16,
2008
The New York Times
To the
Editor:
Re “Researchers Fail to
Reveal Full Drug Pay” (front page, June 8) and “Hidden Drug Payments at
Harvard” (editorial, June 10):
The first obligations of those who conduct lifesaving research at American
medical schools, teaching hospitals and research universities are to protect the
safety of patients and assure the integrity and objectivity of science.
Researchers and their institutions must reveal to research participants
potential financial conflicts of interest and comply with reporting
requirements.
Our associations’ recent report, “Protecting Patients, Preserving Integrity,
Advancing Health,” urges our medical schools and research universities to
require clinical research faculty to report all outside income directly or
indirectly related to professional responsibilities.
The report also strongly urges our institutions to develop and carry out
rigorous oversight policies for institutional conflicts of interest.
The public must be assured that scientific results are honest and that patient
safety is not compromised for financial gain. We are committed to these
principles and hope to work with Senators Charles E. Grassley and Herb Kohl in
their legislative effort.
Robert M. Berdahl
Darrell G. Kirch
Washington, June 11, 2008
The writers are presidents of, respectively, the Association of American
Universities and the Association of American Medical Colleges.
•
To the Editor:
The public deserves to have access to information about relationships between
medicine and the pharmaceutical industry (“Hidden Drug Payments at Harvard,”
editorial, June 10), just as the public should be aware of relationships between
legislators and lobbyists.
Once we know about relationships, we can consider whether any potential
conflicts they pose affect our own interests.
These relationships can have positive outcomes. Financing for much of the
research that has allowed rapid advances in diagnosing and treating illnesses
comes from the same pharmaceutical companies and device makers that profit when
the research is successful. Often medical schools depend on income from this
industry-backed research to educate the next generation of physicians.
The American Psychiatric Association supports and encourages the full disclosure
of relationships between physicians and pharmaceutical companies and any other
possible sources of conflicts of interest. Transparency helps to protect medical
education, research and care.
But for real solutions, we have to look even further to ourselves and to our
government to pay for the kind of medical education and research that has for
decades provided new and better treatments for medical conditions.
Nada Stotland
Chicago, June 11, 2008
The writer, a medical doctor, is president of the American Psychiatric
Association.
•
To the Editor:
Re “Hidden Drug Payments at Harvard” (editorial, June 10):
While it is good news that there is a bill introduced in the Senate that would
require “drug and device makers” to disclose payments to doctors that exceed
$500 annually, such disclosure should also be easily accessible to parents and
other consumers.
In New York, a parent’s informed consent is required before a doctor can
administer nonemergency psychotropic drugs to a child. In order to make a fully
informed choice, parents must be aware of all the relevant information, which
should include a doctor’s potential conflict of interest.
Lawyers are bound to disclose potential conflicts of interest because they may
compromise the lawyer’s professional integrity. Doctors should be held to the
same standard, especially where the lives of children are at stake.
Diane Goldstein Temkin
New York, June 10, 2008
The writer is a lawyer with the Mental Hygiene Legal Service, a state agency
that protects the rights of the mentally disabled.
•
To the Editor:
Re “Researchers Fail to Reveal Full Drug Pay” (front page, June 8):
The Child and Adolescent Bipolar Foundation supports full disclosure of
pharmaceutical company payments to physicians and researchers. Parents and
doctors need all the information to evaluate research on treatments, including
information about potential conflicts.
Families living with pediatric bipolar disorder face challenges few others can
imagine. Their children may be suicidal or explosive and unable to function in
school or at home.
Early treatment saves lives and improves the long-term prognosis, but diagnosis
typically trails onset by a decade. We cannot allow controversy or confusion to
further harm children yet undiagnosed.
Complex psychiatric conditions like pediatric bipolar disorder require more
well-designed, large-scale and long-term studies. These studies should be
federally financed, so researchers will be less reliant on pharmaceutical
financing.
Susan Resko
Exec. Dir., Child and Adolescent
Bipolar Foundation
Wilmette, Ill., June 8, 2008
Doctors, Research and Drug Payments, NYT, 16.6.2008,
http://www.nytimes.com/2008/06/16/opinion/l16drug.html
Editorial
Hidden
Drug Payments at Harvard
June 10,
2008
The New York Times
Three
prominent psychiatrists at the Harvard Medical School and its affiliated
Massachusetts General Hospital have been caught vastly underreporting their
income from drug companies whose fortunes could be affected by their studies and
their promotional efforts on behalf of aggressive drug treatments. Their failure
to divulge their conflicts is striking proof that today’s requirements for
reporting payments from industry — essentially an honor system in which
researchers are supposed to reveal their outside income to their institutions —
needs to be strengthened.
What makes this case particularly troublesome is that the Harvard group’s
research has helped fuel an explosion in the use of powerful antipsychotic drugs
to treat children, as was described in The Times on Sunday by Gardiner Harris
and Benedict Carey. Although supporters praise the most prominent of the trio,
Dr. Joseph Biederman, as a visionary who has saved many lives, critics complain
that the Harvard studies have been too small and loosely designed to provide
conclusive results. Critics say they also were subject to biased interpretation
through use of a subjective rating scale.
The previously unknown payments to the researchers were pried loose by Senator
Charles Grassley of Iowa, the ranking Republican on the Senate Finance
Committee, whose staff reviewed what the researchers disclosed on
conflict-of-interest forms at their institutions and prodded the university to
verify the data as accurate. Under pressure, two of the researchers acknowledged
receiving $1.6 million apiece in consulting fees from drug companies between
2000 and 2007 and the third reported earning more than $1 million. That was far
more than the researchers had originally reported, a number that Mr. Grassley
pegged at a couple hundred thousand dollars apiece. Even the updated numbers
left out other payments that drug companies reported separately that they had
made to the trio.
At this point, it is not clear whether the researchers inadvertently failed to
comply with reporting rules or consciously sought to hide their sizable incomes
from drug companies. But it is clear that relying on researchers to report their
outside incomes and on universities and hospitals to police the disclosures
won’t suffice. Senator Grassley and Senator Herb Kohl, Democrat of Wisconsin,
have introduced a bill that would require drug and device makers to report
annually any payments to doctors that exceed $500 a year. That is the best way
to ensure that conflicts of interest are transparent to all.
Hidden Drug Payments at Harvard, NYT, 10.6.2008,
http://www.nytimes.com/2008/06/10/opinion/10tue2.html?ref=opinion
Researchers Fail to Reveal
Full Drug Pay
June 8,
2008
The New York Times
By GARDINER HARRIS and BENEDICT CAREY
A
world-renowned Harvard child psychiatrist whose work has helped fuel an
explosion in the use of powerful antipsychotic medicines in children earned at
least $1.6 million in consulting fees from drug makers from 2000 to 2007 but for
years did not report much of this income to university officials, according to
information given Congressional investigators.
By failing to report income, the psychiatrist, Dr. Joseph Biederman, and a
colleague in the psychiatry department at Harvard Medical School, Dr. Timothy E.
Wilens, may have violated federal and university research rules designed to
police potential conflicts of interest, according to Senator Charles E.
Grassley, Republican of Iowa. Some of their research is financed by government
grants.
Like Dr. Biederman, Dr. Wilens belatedly reported earning at least $1.6 million
from 2000 to 2007, and another Harvard colleague, Dr. Thomas Spencer, reported
earning at least $1 million after being pressed by Mr. Grassley’s investigators.
But even these amended disclosures may understate the researchers’ outside
income because some entries contradict payment information from drug makers, Mr.
Grassley found.
In one example, Dr. Biederman reported no income from Johnson & Johnson for 2001
in a disclosure report filed with the university. When asked to check again, he
said he received $3,500. But Johnson & Johnson told Mr. Grassley that it paid
him $58,169 in 2001, Mr. Grassley found.
The Harvard group’s consulting arrangements with drug makers were already
controversial because of the researchers’ advocacy of unapproved uses of
psychiatric medicines in children.
In an e-mailed statement, Dr. Biederman said, “My interests are solely in the
advancement of medical treatment through rigorous and objective study,” and he
said he took conflict-of-interest policies “very seriously.” Drs. Wilens and
Spencer said in e-mailed statements that they thought they had complied with
conflict-of-interest rules.
John Burklow, a spokesman for the National Institutes of Health, said: “If there
have been violations of N.I.H. policy — and if research integrity has been
compromised — we will take all the appropriate action within our power to hold
those responsible accountable. This would be completely unacceptable behavior,
and N.I.H. will not tolerate it.”
The federal grants received by Drs. Biederman and Wilens were administered by
Massachusetts General Hospital, which in 2005 won $287 million in such grants.
The health institutes could place restrictions on the hospital’s grants or even
suspend them altogether.
Alyssa Kneller, a Harvard spokeswoman, said in an e-mailed statement: “The
information released by Senator Grassley suggests that, in certain instances,
each doctor may have failed to disclose outside income from pharmaceutical
companies and other entities that should have been disclosed.”
Ms. Kneller said the doctors had been referred to a university conflict
committee for review.
Mr. Grassley sent letters on Wednesday to Harvard and the health institutes
outlining his investigators’ findings, and he placed the letters along with his
comments in The Congressional Record.
Dr. Biederman is one of the most influential researchers in child psychiatry and
is widely admired for focusing the field’s attention on its most troubled young
patients. Although many of his studies are small and often financed by drug
makers, his work helped to fuel a controversial 40-fold increase from 1994 to
2003 in the diagnosis of pediatric bipolar disorder, which is characterized by
severe mood swings, and a rapid rise in the use of antipsychotic medicines in
children. The Grassley investigation did not address research quality.
Doctors have known for years that antipsychotic drugs, sometimes called major
tranquilizers, can quickly subdue children. But youngsters appear to be
especially susceptible to the weight gain and metabolic problems caused by the
drugs, and it is far from clear that the medications improve children’s lives
over time, experts say.
In the last 25 years, drug and device makers have displaced the federal
government as the primary source of research financing, and industry support is
vital to many university research programs. But as corporate research executives
recruit the brightest scientists, their brethren in marketing departments have
discovered that some of these same scientists can be terrific pitchmen.
To protect research integrity, the National Institutes of Health require
researchers to report to universities earnings of $10,000 or more per year, for
instance, in consulting money from makers of drugs also studied by the
researchers in federally financed trials. Universities manage financial
conflicts by requiring that the money be disclosed to research subjects, among
other measures.
The health institutes last year awarded more than $23 billion in grants to more
than 325,000 researchers at over 3,000 universities, and auditing the potential
conflicts of each grantee would be impossible, health institutes officials have
long insisted. So the government relies on universities.
Universities ask professors to report their conflicts but do almost nothing to
verify the accuracy of these voluntary disclosures.
“It’s really been an honor system thing,” said Dr. Robert Alpern, dean of Yale
School of Medicine. “If somebody tells us that a pharmaceutical company pays
them $80,000 a year, I don’t even know how to check on that.”
Some states have laws requiring drug makers to disclose payments made to
doctors, and Mr. Grassley and others have sponsored legislation to create a
national registry.
Lawmakers have been concerned in recent years about the use of unapproved
medications in children and the influence of industry money.
Mr. Grassley asked Harvard for the three researchers’ financial disclosure
reports from 2000 through 2007 and asked some drug makers to list payments made
to them.
“Basically, these forms were a mess,” Mr. Grassley said in comments he entered
into The Congressional Record on Wednesday. “Over the last seven years, it
looked like they had taken a couple hundred thousand dollars.”
Prompted by Mr. Grassley’s interest, Harvard asked the researchers to re-examine
their disclosure reports.
In the new disclosures, the trio’s outside consulting income jumped but was
still contradicted by reports sent to Mr. Grassley from some of the companies.
In some cases, the income seems to have put the researchers in violation of
university and federal rules.
In 2000, for instance, Dr. Biederman received a grant from the National
Institutes of Health to study in children Strattera, an Eli Lilly drug for
attention deficit disorder. Dr. Biederman reported to Harvard that he received
less than $10,000 from Lilly that year, but the company told Mr. Grassley that
it paid Dr. Biederman more than $14,000 in 2000, Mr. Grassley’s letter stated.
At the time, Harvard forbade professors from conducting clinical trials if they
received payments over $10,000 from the company whose product was being studied,
and federal rules required such conflicts to be managed.
Mr. Grassley said these discrepancies demonstrated profound flaws in the
oversight of researchers’ financial conflicts and the need for a national
registry. But the disclosures may also cloud the work of one of the most
prominent group of child psychiatrists in the world.
In the past decade, Dr. Biederman and his colleagues have promoted the
aggressive diagnosis and drug treatment of childhood bipolar disorder, a mood
problem once thought confined to adults. They have maintained that the disorder
was underdiagnosed in children and could be treated with antipsychotic drugs,
medications invented to treat schizophrenia.
Other researchers have made similar assertions. As a result, pediatric bipolar
diagnoses and antipsychotic drug use in children have soared. Some 500,000
children and teenagers were given at least one prescription for an antipsychotic
in 2007, including 20,500 under 6 years of age, according to Medco Health
Solutions, a pharmacy benefit manager.
Few psychiatrists today doubt that bipolar disorder can strike in the early
teenage years, or that many of the children being given the diagnosis are deeply
distressed.
“I consider Dr. Biederman a true visionary in recognizing this illness in
children,” said Susan Resko, director of the Child and Adolescent Bipolar
Foundation, “and he’s not only saved many lives but restored hope to thousands
of families across the country.”
Longtime critics of the group see its influence differently. “They have given
the Harvard imprimatur to this commercial experimentation on children,” said
Vera Sharav, president and founder of the Alliance for Human Research
Protection, a patient advocacy group.
Many researchers strongly disagree over what bipolar looks like in youngsters,
and some now fear the definition has been expanded unnecessarily, due in part to
the Harvard group.
The group published the results of a string of drug trials from 2001 to 2006,
but the studies were so small and loosely designed that they were largely
inconclusive, experts say. In some studies testing antipsychotic drugs, the
group defined improvement as a decline of 30 percent or more on a scale called
the Young Mania Rating Scale — well below the 50 percent change that most
researchers now use as the standard.
Controlling for bias is especially important in such work, given that the scale
is subjective, and raters often depend on reports from parents and children,
several top psychiatrists said.
More broadly, they said, revelations of undisclosed payments from drug makers to
leading researchers are especially damaging for psychiatry.
“The price we pay for these kinds of revelations is credibility, and we just
can’t afford to lose any more of that in this field,” said Dr. E. Fuller Torrey,
executive director of the Stanley Medical Research Institute, which finances
psychiatric studies. “In the area of child psychiatry in particular, we know
much less than we should, and we desperately need research that is not
influenced by industry money.”
Researchers Fail to Reveal Full Drug Pay, NYT, 8.6.2008,
http://www.nytimes.com/2008/06/08/us/08conflict.html?ref=opinion
A City
Where Hospitals Are as Ill as the Patients
June 5,
2008
The New York Times
By JENNIFER STEINHAUER
LOS ANGELES
— The patients line up at 6:30 a.m. outside the tidy clinic. Two hours later,
when it opens, they will sit and wait some more.
There are 22-year-olds, holding neat piles of pills on their laps, small
children whose mothers try to distract them with plastic rattles, elderly
immigrants who sit silently, staring at nothing in particular, until their names
are called.
And there are nearly 70 percent more of them walking into the clinic, the St.
John’s Well Child and Family Center in Compton, since nearby Martin Luther King
Jr.-Harbor Hospital closed last summer.
For thousands of residents of South Los Angeles who had depended on the large
county-run King-Harbor hospital, the past 10 months have been a grueling
exercise in cobbling together medical care. When King-Harbor was shut by federal
officials, it became the 15th general acute care hospital to close in Los
Angeles County since 2000, about half of which served residents in South Los
Angeles.
The loss of King-Harbor was less a seminal moment than another episode in the
continuing health care ordeal among this city’s sickest and poorest residents.
South Los Angeles is one of the most difficult places in the nation to both
receive and give medical care. Family doctors are few and far between, and the
area is one of the hardest to draw new doctors to, physician recruiters say.
Chronically ill residents say they never quite know what a call to 911 will
yield.
“You call an ambulance and you think you’re going to St. Francis and they say
it’s full,” said Denise Provost, whose largely untreated asthma routinely sends
her to the emergency room. “So they take you to Kaiser. If that’s full, then
it’s Long Beach. You go way out of your way.”
Julia Villalobos, among those waiting at St. John’s one recent morning, heads to
a different clinic in Long Beach when she is sick. She takes her mother, who
suffers seizures, to St. Francis Medical Center in neighboring Lynwood. And when
her two young sons need checkups, she parks herself at St. John’s.
“They are good here,” Ms. Villalobos said. “They explain everything really
good.”
The vast majority of residents in central Los Angeles are uninsured or are on
the state’s Medicaid program — known as Medical — which offers the lowest
reimbursement rates in the nation, and a growing population of illegal
immigrants who are not eligible for government insurance have flooded the ranks
of the uninsured.
Gov. Arnold Schwarzenegger, a Republican, has proposed another 10 percent cut in
the state’s Medicaid program to balance the state’s budget while Congress
contemplates a host of reductions to the program that, if approved, would mean
$240 million less for Los Angeles.
Los Angeles County’s health department, the provider of last resort, is sagging
under its own budget woes, and it adopted complex patient-transfer policies that
have shifted an increasing number of its indigent patients to private hospitals,
which are in barely better financial shape.
“We have an all-out crisis here,” said Carol Meyer, the director of governmental
relations for the Los Angeles County Health Services Department. “In terms of
lack of access to care, emergency room overcrowding and total underfunding of
the health care system.”
In many ways, the woes of South Los Angeles mirror other poor urban health care
systems. Medical centers in Philadelphia, Washington, Cleveland and elsewhere
have closed or fallen into bankruptcy in recent years, leaving patients
scrambling.
Also, Medicaid reductions in recent years have helped contribute to the rising
tide of the uninsured — roughly 2.2 million more in 2006 than in the previous
year — largely because of a decrease in employer-sponsored insurance and
Medicaid reductions.
“Over the course of the last 10 to 15 years, there are entire populations that
have been wiped off Medicaid,” said Larry S. Gage, president of the National
Association of Public Hospitals.
But even against that backdrop, the situation in South Los Angeles is
particularly grave. Most strikingly, the state Medicaid program offers the
lowest reimbursement rate per capita in the nation, nearly 12 percent less than
the second lowest-paying state, Arizona, according to 2005 figures.
Roughly 14 percent of the nation’s uninsured live in California, and one in
three visits to a Los Angeles emergency room are made by someone without
insurance. Many of those patients have conditions that have gone untreated for
months and need to be admitted, further straining hospital resources.
From 2000 to 2006, the number of Medicaid-covered patients using the South Los
Angeles hospitals on Medicaid increased 18 percent and the uninsured ranks rose
more than 20 percent, while patients with commercial coverage fell 20 percent,
according to the hospital association’s figures.
As a result, many hospitals in the South Los Angeles area are unable to stay
afloat, and centers that once served 100,000 patients here have closed.
“I don’t think we have seen that many closures occur in any part of the U.S. in
the last 25 years,” said Jim Lott, vice president of the Hospital Association of
Southern California. “We have less than one hospital bed per 1,000 residents
here compared to 4.3 per 1,000 in the U.S. When you add up all the forces, the
price of indigent care is putting people over the edge.”
King-Harbor hospital, as it has been known in recent years, opened after the
Watts riots in 1965, and quickly became a jewel of the largely minority
community, serving as a medical home for many and a steady source of employment
for black doctors and local residents. But in recent years the hospital had been
found to have myriad management and quality problems, including patient deaths
that health officials said were related to poor care.
The hospital shut down last August after federal regulators found the center was
out of compliance in 8 of 23 conditions. (The state has been looking for a
private operator to reopen the hospital, but has found no takers.) Only an
outpatient clinic remained, leaving Watts and other neighboring communities
without an emergency room for several miles.
While nine hospitals in the area are officially considered “impacted” by the
closing of King-Harbor, the closest, St. Francis Medical Center, has clearly
taken on much of the burden. Its emergency room has added 14 beds, for a total
of 46, as the number of patients has increased to almost 180 a day, from about
155, since King-Harbor closed.
St. Francis’s intensive care unit once had about 26 patients on any given day;
it now houses about 33, which has greatly strained the staff, said Gerald Kozai,
the hospital’s president.
“All of us would say it has probably been our most challenging year,” Mr. Kozai
said.
And it has gotten harder to find help. South Los Angeles is rated 9 on a scale
of 10 of undesirable places for doctors to work, said Phil Miller, a spokesman
for Merritt Hawkins & Associates, a large physician recruiting firm. “It has
become fairly well known in the physician community that the Medical
reimbursement rate is not good, and you add the negative publicity from the
closures there,” and few doctors are willing to step in, Mr. Miller said.
After it closed, King-Harbor maintained a clinic that set a target of 190,000
visits a year, but it is falling well below that goal. On a recent visit, the
waiting room was nearly empty, while the St. John’s clinic was filled.
Health care providers and patients said King-Harbor’s reputation for poor care
had sent patients to other emergency rooms or area clinics. “It has a bad
reputation,” Ms. Villalobos said. “I wouldn’t want to go there.”
Indeed, area clinics have been absorbing needy patients. Among the nine clinics
run by St. John’s, there has been a 157 percent increase in visits since
King-Harbor closed, said Jim Mangia, who runs the consortium.
The clinics provide free or low-cost health care to its patients — 65 percent of
whom are uninsured — via subsidies from grants and money distributed by the
county beginning in July. Those funds usually get the clinics through most of
the year, but the St. John’s clinic in Compton ran out in February.
“Community clinics are picking up the slack and not getting reimbursed from
those services,” Mr. Mangia said, “and many community clinics are teetering on
the brink of insolvency.”
If patients are not using King-Harbor’s clinic, its emergency room is missed. “I
know they called it Killer King, but they always took good care of me,” said
Lionel Waller, a lifelong resident of Watts.
Mr. Waller, like others in the neighborhood, said that since the hospital
closed, seriously injured people had to be taken to centers 10 to 15 miles away,
including a friend of his who recently died of a gunshot wound.
“I keep wondering if they would have taken him some place closer if he would
have made it,” Mr. Waller said. “We need that hospital here.”
A City Where Hospitals Are as Ill as the Patients, NYT,
5.6.2008,
http://www.nytimes.com/2008/06/05/us/05southla.html?hp
More
than 2 million U.S. youths depressed: study
Tue May 13,
2008
2:17pm EDT
Reuters
WASHINGTON
(Reuters) - More than 2 million U.S. teenagers have suffered a serious bout of
depression in the past year, including nearly 13 percent of girls, according to
a federal government survey released on Tuesday.
On average, 8.5 percent of adolescents aged 12 to 17 described having had a
major depressive episode in the previous year, the Substance Abuse and Mental
Health Services Administration reported.
But there were "striking differences" by sex, with 12.7 percent of girls and 4.6
percent of boys affected.
Depression is the leading cause of suicide, which in turn is the third-leading
cause of death for 15- to 24-year-olds in the United States.
"Combined 2004 to 2006 data show that rates of past year major depressive
episode among youths aged 12 to 17 generally increased with increasing age," the
researchers wrote.
Researchers at SAMHSA and RTI International in Research Triangle Park, North
Carolina, prepared the report using data from the National Survey on Drug Use
and Health.
More than 67,700 youths aged 12 to 17 answered questions about mood and
depression. They were also asked to rate how depression affected them using the
Sheehan Disability Scale, which measures impact on family, friends, chores at
home, work and school.
They defined a major depressive episode as two weeks or longer of depressed mood
or loss of interest or pleasure, and at least four other symptoms such as
problems with sleep, energy, concentration or self-image.
Nearly half of the teenagers who had major depression said it severely impaired
their ability to function in at least one of the areas on the disability scale.
The worst cases were unable to carry out normal activities for an average of 58
days in the past year.
"Fortunately, depression responds very well to early intervention and
treatment," SAMHSA Administrator Terry Cline said in a statement.
"Parents concerned about their child's mental health should seek help with the
same urgency as with any other medical condition. Appropriate mental health care
can help their child recover and thrive."
(Reporting by Maggie Fox; Editing by John O'Callaghan)
More than 2 million U.S. youths depressed: study, R,
13.5.2008,
http://www.reuters.com/article/newsOne/idUSN1340857020080513
Rough
Transition to a New Asthma Inhaler
May 13,
2008
The New York Times
By LAURIE TARKAN
Millions of
people with asthma and other lung diseases will have to switch inhalers by the
end of the year. And for many, the transition will not be smooth.
The change — mandated by the federal government in 2005, to go into effect next
Jan. 1 — is to comply with the 1987 treaty to protect the earth’s ozone layer.
It bans most uses of chlorofluorocarbons, or CFCs, which are used as propellants
in many inhalers.
CFC-free inhalers have been available for more than a decade. But four million
to five million users have yet to switch, according to the consumer advocacy
group Allergy and Asthma Network Mothers of Asthmatics.
For one thing, the old inhalers cost much less — an average of $13.50, or
one-third the price of a CFC-free inhaler, which uses propellants called HFAs,
for hydrofluoroalkanes. (CFC inhalers are generic; HFA inhalers are brand-name.)
People with asthma use an average of three or four inhalers a year, but some
patients use one a month.
Moreover, the new and old inhalers differ in feel, force and taste, and how they
are primed and cleaned. Advocates for people with asthma say doctors and
patients have not been educated about the changes.
“What the government failed to do is to mandate anyone to tell patients and
physicians this transition was happening,” said Nancy Sander, president of the
asthma group. “There is no education, no monitoring of patients, no financial
assistance to patients who have to pay higher prices for the new drugs.”
As a result, she and others say, there have been unnecessary fears about the
newer inhalers, preventable trips to the emergency room and even some hoarding
of CFC inhalers.
Callers to a hot line run by Ms. Sander’s group have complained that when they
were switched to the new inhalers, the differences between the two types were
never explained. Many thought that their device was broken or that their
symptoms were not being relieved by the new inhalers.
The Food and Drug Administration says that since January 2007 it has received
415 complaints about HFA inhalers’ costing too much or not working properly.
After a public meeting last month in which doctors and patients said most people
were unaware of the transition, the agency has been stepping up educational
efforts, with several public service announcements expected by the end of this
month, said Deborah Henderson, an official at the Center for Drug Evaluation and
Research.
Both types of inhalers use albuterol, a short-acting medication that can prevent
an asthma attack when used preventively — before exercising, for example — or at
the first sign of breathing trouble.
But the cost difference has meant huge gains for drug companies. As people
switched to HFA inhalers in 2006 and 2007, sales of all albuterol inhalers
jumped from about $500 million to $1.1 billion, according to I.M.S. Health, a
health care information company. Of the 40.5 million prescriptions written for
albuterol inhalers last year, it said, about half were CFC and half were HFA
inhalers.
And even though there are important differences between the four brands of HFA
inhalers, some insurers cover only one of the four. Advocates say the higher
cost may keep patients from buying inhalers or force them to cut back on other
medications or switch to a less effective over-the-counter inhaler that uses
epinephrine.
Several members of Congress are asking the Bush administration to require
insurers, including the Medicare and Medicaid programs, to cover the new
inhalers equally. Representative Steve Kagen, a Wisconsin Democrat who is also
an allergy and asthma physician, said it was important “to make sure there’s as
little co-pay as possible.”
The four HFA inhalers are Ventolin by GlaxoSmithKline, ProAir by Ivax, Proventil
by Schering-Plough and Xopenex by Sepracor. (Xopenex uses a different chemical,
levalbuterol.) All companies have give-away programs for those in need and are
providing free samples that doctors give to their patients. There is also
financial assistance available through the Partnership for Prescription
Assistance (1-888-477-2669).
Studies show that HFA inhalers are as effective as CFC inhalers and have the
same rate of side effects. But if they are not used properly, patients will not
get adequate doses. There are three critical differences.
HFA inhalers must be pumped four times to prime them — a number that was not so
critical with the more forgiving CFC inhalers, said Dr. Leslie Hendeles,
professor of pharmacy and pediatrics at the University of Florida. And each
brand of the newer inhaler requires a different frequency of priming.
HFA inhalers have a weaker spray. “It’s very soft so people think it’s not
working,” Dr. Stoloff said. Where CFC inhalers deliver a powerful force that
feels as if the airway is being pushed open, the newer ones provide a warm, soft
mist that also has a distinct taste.
They also require a slower inhale. “You have to take a nice slow, deep breath
and hold it,” Ms. Sander said. If people worry that it’s not working, they may
not take the second puff, may fail to wait the necessary 30 seconds between
puffs or may take too many puffs. ,And their anxiety may rise, further
constricting their airways.
HFA inhalers need to be washed with warm water and air dried once a week. The
medication is stickier and will clog the hole, reducing the amount of medication
the spray delivers.
There are also important differences among the brands, though some doctors
simply write Albuterol HFA on the prescription, leaving the pharmacist to choose
the brand. Only one, Ventalin, has a dose counter, which helps users keep track
of how much medication is left. ProAir appears to be on many insurance
companies’ lists of approved medications, but it has the softest spray, Dr.
Stoloff said.
Rough Transition to a New Asthma Inhaler, NYT, 13.5.2008,
http://www.nytimes.com/2008/05/13/health/13asth.html
|