|
History > 2008 > USA > Health (VI)
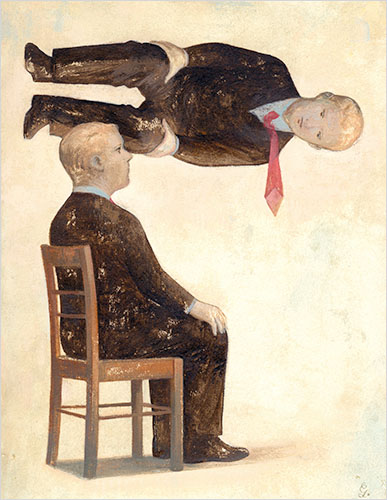
Illustration: Gerard Dubois
NYT
December 1, 2008
Standing in Someone Else’s Shoes, Almost for Real
NYT
2.12.2008
https://www.nytimes.com/2008/12/02/health/02mind.html
Expansion of Clinics
Shapes a Bush Legacy
December 26, 2008
The New York Times
By KEVIN SACK
NASHVILLE — Although the number of uninsured and the cost of coverage have
ballooned under his watch, President Bush leaves office with a health care
legacy in bricks and mortar: he has doubled federal financing for community
health centers, enabling the creation or expansion of 1,297 clinics in medically
underserved areas.
For those in poor urban neighborhoods and isolated rural areas, including Indian
reservations, the clinics are often the only dependable providers of basic
services like prenatal care, childhood immunizations, asthma treatments, cancer
screenings and tests for sexually transmitted diseases.
As a crucial component of the health safety net, they are lauded as a
cost-effective alternative to hospital emergency rooms, where the uninsured and
underinsured often seek care.
Despite the clinics’ unprecedented growth, wide swaths of the country remain
without access to affordable primary care. The recession has only magnified the
need as hundreds of thousands of Americans have lost their employer-sponsored
health insurance along with their jobs.
In response, Democrats on Capitol Hill are proposing even more significant
increases, making the centers a likely feature of any health care deal struck by
Congress and the Obama administration.
In Nashville, United Neighborhood Health Services, a 32-year-old community
health center, has seen its federal financing rise to $4.2 million, from $1.8
million in 2001. That has allowed the organization to add eight clinics to its
base of six, and to increase its pool of patients to nearly 25,000 from 10,000.
Still, says Mary Bufwack, the center’s chief executive, the clinics satisfy only
a third of the demand in Nashville’s pockets of urban poverty and immigrant
need.
One of the group’s recent grants helped open the Southside Family Clinic, which
moved last year from a pair of public housing apartments to a gleaming new
building on a once derelict corner.
As she completed a breathing treatment one recent afternoon, Willie Mai Ridley,
a 68-year-old beautician, said she would have sought care for her bronchitis in
a hospital emergency room were it not for the new clinic. Instead, she took a
short drive, waited 15 minutes without an appointment and left without paying a
dime; the clinic would bill her later for her Medicare co-payment of $18.88.
Ms. Ridley said she appreciated both the dignity and the affordability of her
care. “This place is really very, very important to me,” she said, “because you
can go and feel like you’re being treated like a person and get the same medical
care you would get somewhere else and have to pay $200 to $300.”
As governor of Texas, Mr. Bush came to admire the missionary zeal and
cost-efficiency of the not-for-profit community health centers, which qualify
for federal operating grants by being located in designated underserved areas
and treating patients regardless of their ability to pay. He pledged support for
the program while campaigning for president in 2000 on a platform of
“compassionate conservatism.”
In Mr. Bush’s first year in office, he proposed to open or expand 1,200 clinics
over five years (mission accomplished) and to double the number of patients
served (the increase has ended up closer to 60 percent). With the health centers
now serving more than 16 million patients at 7,354 sites, the expansion has been
the largest since the program’s origins in President Lyndon B. Johnson’s war on
poverty, federal officials said.
“They’re an integral part of a health care system because they provide care for
the low-income, for the newly arrived, and they take the pressure off of our
hospital emergency rooms,” Mr. Bush said last year while touring a clinic in
Omaha.
With federal encouragement, the centers have made a major push this decade to
expand dental and mental health services, open on-site pharmacies, extend hours
to nights and weekends and accommodate recent immigrants — legal and otherwise —
by employing bilingual staff. More than a third of patients are now Hispanic,
according to the National Association of Community Health Centers.
The centers now serve one of every three people who live in poverty and one of
every eight without insurance. But a study released in August by the Government
Accountability Office found that 43 percent of the country’s medically
underserved areas lack a health center site. The National Association of
Community Health Centers and the American Academy of Family Physicians estimated
last year that 56 million people were “medically disenfranchised” because they
lived in areas with inadequate primary care.
President-elect Barack Obama has said little about how the centers may fit into
his plans to remake American health care. But he was a sponsor of a Senate bill
in August that would quadruple federal spending on the program — to $8 billion
from $2.1 billion — and increase incentives for medical students to choose
primary care. His wife, Michelle, worked closely with health centers in Chicago
as vice president for community and external relations at the University of
Chicago Medical Center.
And Mr. Obama’s choice to become secretary of health and human services, former
Senator Tom Daschle of South Dakota, argues in his recent book on health care
that financing should be increased, describing the health centers as “a
godsend.”
The federal program, which was first championed in Congress by Senator Edward M.
Kennedy, Democrat of Massachusetts, has earned considerable bipartisan support.
Leading advocates, like Senator Bernie Sanders, independent of Vermont, and
Representative James E. Clyburn, Democrat of South Carolina, the House majority
whip, argue that any success Mr. Obama has in reducing the number of uninsured
will be meaningless if the newly insured cannot find medical homes. In
Massachusetts, health centers have seen increased demand since the state began
mandating health coverage two years ago.
At $8 billion, the Senate measure may be considered a relative bargain compared
with the more than $100 billion needed for Mr. Obama’s proposal to subsidize
coverage for the uninsured. If his plan runs into fiscal obstacles, a vast
expansion of community health centers may again serve as a stopgap while
universal coverage waits for flusher times.
Recent job losses, meanwhile, are stoking demand for the clinics’ services,
often from first-time users. The United Neighborhood Health Services clinics in
Nashville have seen a 35 percent increase in patients this year, with much of
the growth from the newly jobless.
“I’m seeing a lot of professionals that no longer have their insurance or
they’re laid off from their jobs,” said Dr. Marshelya D. Wilson, a physician at
the center’s Cayce clinic. “So they come here and get their health care.”
Studies have generally shown that the health centers — which must be governed by
patient-dominated boards — are effective at reducing racial and ethnic
disparities in medical treatment and save substantial sums by keeping patients
out of hospitals. Their trade association estimates that they save the health
care system $17.6 billion a year, and that an equivalent amount could be saved
if avoidable emergency room visits were diverted to clinics. Some centers,
including here in Nashville, have brokered agreements with hospitals to do
exactly that.
Many centers are finding that federal support is not keeping pace with the
growing cost of treating the uninsured. Government grants now account for 19
percent of community health center revenues, compared with 22 percent in 2001,
according to the Health Resources and Services Administration, which oversees
the program. The largest revenue sources are public insurance plans like
Medicaid, Medicare and the State Children’s Health Insurance Program, making the
centers vulnerable to government belt-tightening.
The centers are known for their efficiency. Though United Neighborhood Health
Services has more than doubled in size this decade, Ms. Bufwack, its chief
executive, manages to run five neighborhood clinics, five school clinics, a
homeless clinic, two mobile clinics and a rural clinic, with 24,391 patients, on
a budget of $8.1 million. Starting pay for her doctors is $120,000. Patients are
charged on an income-based sliding scale, and the uninsured are expected to pay
at least $20 for an office visit. One clinic is housed in a double-wide trailer.
Because of a nationwide shortage of primary care physicians, the clinics rely on
federal programs like the National Health Service Corps that entice medical
students with grants and loan write-offs in exchange for agreements to practice
as generalists in underserved areas. Of the 16 doctors working for United
Neighborhood, seven are current or former participants.
Dr. LaTonya D. Knott, 37, who treated Ms. Ridley for her bronchitis, is among
them. Born to a 15-year-old mother in south Nashville, she herself had been a
regular childhood patient at one of the center’s clinics. After graduating as
her high school’s valedictorian, she went to college on scholarships and then to
medical school on government grants, with an obligation to serve for two years.
She said she now felt a responsibility to be a role model. “I do a whole lot of
social work,” she said, noting that it was not uncommon for children to drop by
the clinic for help with homework, or for a peanut butter sandwich. “It’s not
just that we provide the medical care. I’m trying to provide you with a future.”
Despite such commitment, national staffing shortages have reinforced concerns
about the quality of care at health centers, notably the management of chronic
diseases. This year, the government started collecting data at the centers on
performance measures like cervical cancer screening and diabetes control.
“The question is not just, ‘Are you going to have more community health
centers?’ ” said Dr. H. Jack Geiger, founder of the health centers movement and
a professor emeritus at the City University of New York. “It’s, ‘Are you going
to have adequate services?’ ”
A deeper frustration for health centers concerns their difficulty in securing
follow-up appointments with specialists for patients who are uninsured or have
Medicaid. All too often, said Ms. Bufwack, medical care ends at the clinic door,
reinforcing the need to expand both primary care and health insurance coverage.
“That’s when our doctors feel they’re practicing third world medicine,” she
said. “You will die if you have cancer or a heart condition or bad asthma or
horrible diabetes. If you need a specialist and specialty tests and specialty
meds and specialty surgery, those things are totally out of your reach.”
Expansion of Clinics
Shapes a Bush Legacy, NYT, 26.12.2008,
http://www.nytimes.com/2008/12/26/health/policy/26clinics.html
Psychiatrists
Revising the
Book of Human Troubles
December 18, 2008
The New York Times
By BENEDICT CAREY
The book is at least three
years away from publication, but it is already stirring bitter debates over a
new set of possible psychiatric disorders.
Is compulsive shopping a mental problem? Do children who continually recoil from
sights and sounds suffer from sensory problems — or just need extra attention?
Should a fetish be considered a mental disorder, as many now are?
Panels of psychiatrists are hashing out just such questions, and their answers —
to be published in the fifth edition of the Diagnostic and Statistical Manual of
Mental Disorders — will have consequences for insurance reimbursement, research
and individuals’ psychological identity for years to come.
The process has become such a contentious social and scientific exercise that
for the first time the book’s publisher, the American Psychiatric Association,
has required its contributors to sign a nondisclosure agreement.
The debate is particularly intense because the manual is both a medical
guidebook and a cultural institution. It helps doctors make a diagnosis and
provides insurance companies with diagnostic codes without which the insurers
will not reimburse patients’ claims for treatment.
The manual — known by its initials and edition number, DSM-V — often organizes
symptoms under an evocative name. Labels like obsessive-compulsive disorder have
connotations in the wider culture and for an individual’s self-perception.
“This is not cardiology or nephrology, where the basic diseases are well known,”
said Edward Shorter, a leading historian of psychiatry whose latest book,
“Before Prozac,” is critical of the manual. “In psychiatry no one knows the
causes of anything, so classification can be driven by all sorts of factors” —
political, social and financial.
“What you have in the end,” Mr. Shorter said, “is this process of sorting the
deck of symptoms into syndromes, and the outcome all depends on how the cards
fall.”
Psychiatrists involved in preparing the new manual contend that it is too early
to say for sure which cards will be added and which dropped.
The current edition of the manual, which was published in 2000, describes 283
disorders — about triple the number in the first edition, published in 1952.
The scientists updating the manual have been meeting in small groups focusing on
categories like mood disorders and substance abuse — poring over the latest
scientific studies to clarify what qualifies as a disorder and what might
distinguish one disorder from another. They have much more work to do, members
say, before providing recommendations to a 28-member panel that will gather in
closed meetings to make the final editorial changes.
Experts say that some of the most crucial debates are likely to include gender
identity, diagnoses of illness involving children, and addictions like shopping
and eating.
“Many of these are going to involve huge fights, I expect,” said Dr. Michael
First, a professor of psychiatry at Columbia who edited the fourth edition of
the manual but is not involved in the fifth.
One example, Dr. First said, is binge eating, now in the manual’s appendix as a
tentative category.
“A lot of people want that included in the manual,” Dr. First said, “and there’s
some research out there, some evidence that drugs are helpful. But binge eating
is also a normal behavior, and you run the risk of labeling up to 30 percent of
people with a disorder they don’t really have.”
The debate over gender identity, characterized in the manual as “strong and
persistent cross-gender identification,” is already burning hot among
transgender people. Soon after the psychiatric association named the group of
researchers working on sexual and gender identity, advocates circulated online
petitions objecting to two members whose work they considered demeaning.
Transgender people are themselves divided about their place in the manual. Some
transgender men and women want nothing to do with psychiatry and demand that the
diagnosis be dropped. Others prefer that it remain, in some form, because a
doctor’s written diagnosis is needed to obtain insurance coverage for treatment
or surgery.
“The language needs to be reformed, at a minimum,” said Mara Keisling, executive
director of the National Center for Transgender Equity. “Right now, the manual
implies that you cannot be a happy transgender person, that you have to be a
social wreck.”
Dr. Jack Drescher, a New York psychoanalyst and member of the sexual disorders
work group, said that, in some ways, the gender identity debate echoed efforts
to remove homosexuality from the manual in the 1970s.
After protests by gay activists provoked a scientific review, the
“homosexuality” diagnosis was dropped in 1973. It was replaced by “sexual
orientation disturbance” and then “ego-dystonic homosexuality” before being
dropped in 1987.
“You had, in my opinion, what was a social issue, not a medical one; and, in
some sense, psychiatry evolved through interaction with the wider culture,” Dr.
Drescher said.
The American Psychiatric Association says the contributors’ nondisclosure
agreement is meant to allow the revisions to begin without distraction and to
prevent authors from making deals to write casebooks or engage in other projects
based on the deliberations without working through the association.
In a phone interview, Dr. Darrel A. Regier, the psychiatric association’s
research director, who with Dr. David Kupfer of the University of Pittsburgh is
co-chairman of the task force, said that experts working on the manual had
presented much of their work in scientific conferences.
“But you need to synthesize what you’re doing and make it coherent before having
that discussion,” Dr. Regier said. “Nobody wants to put a rough draft or raw
data up on the Web.”
Some critics, however, say the secrecy is inappropriate.
“When I first heard about this agreement, I just went bonkers,” said Dr. Robert
Spitzer, a psychiatry professor at Columbia and the architect of the third
edition of the manual. “Transparency is necessary if the document is to have
credibility, and, in time, you’re going to have people complaining all over the
place that they didn’t have the opportunity to challenge anything.”
Scientists who accepted the invitation to work on the new manual — a prestigious
assignment — agreed to limit their income from drug makers and other sources to
$10,000 a year for the duration of the job. “That’s more conservative” than the
rules at many agencies and universities, Dr. Regier said.
This being the diagnostic manual, where virtually every sentence is likely to be
scrutinized, critics have said that the policy is not strict enough. They have
long suspected that pharmaceutical money subtly influences authors’ decisions.
Industry influence was questioned after a surge in diagnoses of bipolar disorder
in young children. Once thought to affect only adults and adolescents, the
disorder in children was recently promoted by psychiatrists on drug makers’
payrolls.
The team working on childhood disorders is expected to debate the merits of
adding pediatric bipolar as a distinct diagnosis, experts say. It is also
expected to discuss whether Asperger’s syndrome, a developmental disorder,
should be merged with high-functioning autism. The two are virtually identical,
but bear different social connotations.
The same team is likely to make a recommendation on so-called sensory processing
disorder, a vague label for a poorly understood but disabling childhood
behavior. Parent groups and some researchers want recognition in the manual in
order to help raise money for research and obtain insurance coverage of
expensive treatments.
“I know that some are pushing very hard to get that in,” Dr. First said, “and
they believe they have been warmly received. But you just never know for sure,
of course, until the thing is published.”
In all, it is a combination of suspense, mystery and prepublication controversy
that many publishers would die for. The psychiatric association knows it has a
corner on the market and a blockbuster series. The last two editions sold more
than 830,000 copies each.
Psychiatrists Revising the Book of
Human Troubles, NYT, 18.12.2008,
http://www.nytimes.com/2008/12/18/health/18psych.html?hp
Mind
A Crisis of Confidence for Masters of the Universe
December 16, 2008
The New York Times
By RICHARD A. FRIEDMAN, M.D.
Meltdown. Collapse. Depression. Panic. The words would seem to
apply equally to the global financial crisis and the effect of that crisis on
the human psyche.
Of course, it is too soon to gauge the true psychiatric consequences of the
economic debacle; it will be some time before epidemiologists can tell us for
certain whether depression and suicide are on the rise. But there’s no question
that the crisis is leaving its mark on individuals, especially men.
One patient, a hedge fund analyst, came to me recently in a state of great
anxiety. “It’s bad, but it might get a lot worse,” I recall him saying. The
anxiety was expected and appropriate: he had lost a great deal of his (and
others’) assets, and like the rest of us he had no idea where the bottom was. I
would have been worried if he hadn’t been anxious.
Over the course of several weeks, with the help of some anti-anxiety medication,
his panic subsided as he realized that he would most likely survive
economically.
But then something else emerged. He came in one day looking subdued and plopped
down in the chair. “I’m over the anxiety, but now I feel like a loser.” This
from a supremely self-confident guy who was viewed by his colleagues as an
unstoppable optimist.
He was not clinically depressed: his sleep, appetite, sex drive and ability to
enjoy himself outside of work were unchanged. This was different.
The problem was that his sense of success and accomplishment was intimately tied
to his financial status; he did not know how to feel competent or good about
himself without this external measure of his value.
He wasn’t the only one. Over the last few months, I have seen a group of
patients, all men, who experienced a near collapse in their self-esteem, though
none of them were clinically depressed.
Another patient summed it up: “I used to be a master-of-the-universe kind of
guy, but this cut me down to size.”
I have plenty of female patients who work in finance at high levels, but none of
them has had this kind of psychological reaction. I can’t pretend this is a
scientific survey, but I wonder if men are more likely than women to respond
this way. At the risk of trading in gender stereotypes, do men rely
disproportionately more on their work for their self-esteem than women do? Or
are they just more vulnerable to the inevitable narcissistic injury that comes
with performing poorly or losing one’s job?
A different patient was puzzled not by his anxiety about the market, but by his
total lack of self-confidence. He had always had an easy intuitive feel for
finance. But in the wake of the market collapse, he seriously questioned his
knowledge and skill.
Each of these patients experienced a sudden loss of the sense of mastery in the
face of the financial meltdown and could not gauge their success or failure
without the only benchmark they knew: a financial profit.
The challenge of maintaining one’s self-esteem without recognition or reward is
daunting. Chances are that if you are impervious to self-doubt and go on feeling
good about yourself in the face of failure, you have either won the
temperamental sweepstakes or you have a real problem tolerating bad news.
Of course, the relationship between self-esteem and achievement can be circular.
Some argue that that the best way to build self-esteem is to tell people at
every turn how nice, smart and talented they are.
That is probably a bad idea if you think that self-esteem and recognition should
be the result of accomplishment; you feel good about yourself, in part, because
you have done something well. On the other hand, it is hard to imagine people
taking the first step without first having some basic notion of self-confidence.
On Wall Street, though, a rising tide lifts many boats and vice versa, which
means that there are many people who succeed — or fail — through no merit or
fault of their own.
This observation might ease a sense of personal responsibility for the economic
crisis, but it was of little comfort to my patients. I think this is because for
many of them, the previously expanding market gave them a sense of power along
with something as strong as a drug: thrill.
The human brain is acutely attuned to rewards like money, sex and drugs. It
turns out that the way a reward is delivered has an enormous impact on its
strength. Unpredictable rewards produce much larger signals in the brain’s
reward circuit than anticipated ones. Your reaction to situations that are
either better or worse than expected is generally stronger to those you can
predict.
In a sense, the stock market is like a vast gambling casino where the reward can
be spectacular, but always unpredictable. For many, the lure of investing is the
thrill of uncertain reward. Now that thrill is gone, replaced by anxiety and
fear.
My patients lost more than money in the market. Beyond the rush and excitement,
they lost their sense of competence and success. At least temporarily: I have no
doubt that, like the economy, they will recover. But it’s a reminder of just how
fragile our self-confidence can be.
Richard A. Friedman is a professor of psychiatry at Weill Cornell Medical
College.
A Crisis of
Confidence for Masters of the Universe, NYT, 16.12.2008,
http://www.nytimes.com/2008/12/16/health/views/16mind.html
Suits
Over ‘Light’ Cigarettes Allowed
December
15, 2008
Filed at 11:18 a.m. ET
The New York Times
By THE ASSOCIATED PRESS
WASHINGTON
(AP) -- The Supreme Court on Monday handed a surprising defeat to tobacco
companies counting on it to put an end to lawsuits alleging deceptive marketing
of ''light'' cigarettes.
In a 5-4 split won by the court's liberals, it ruled that smokers may use state
consumer protection laws to sue cigarette makers for the way they promote
''light'' and ''low tar'' brands.
The decision was at odds with recent anti-consumer rulings that limited state
regulation of business in favor of federal power.
The tobacco companies argued that the lawsuits are barred by the federal
cigarette labeling law, which forbids states from regulating any aspect of
cigarette advertising that involves smoking and health.
Justice John Paul Stevens, however, said in his majority opinion that the
labeling law does not shield the companies from state laws against deceptive
practices. The decision forces tobacco companies to defend dozens of suits filed
by smokers in Maine, where the case originated, and across the country.
People suing the cigarette makers still must prove that the use of 'light' and
'lowered tar' actually violate the state anti-fraud laws, but those lawsuits may
go forward, Stevens said.
He was joined by the other liberal justices, Stephen Breyer, Ruth Bader Ginsburg
and David Souter, as well as Justice Anthony Kennedy, whose vote often decides
cases where there is an ideological division.
The conservative justices, Chief Justice John Roberts and Justices Samuel Alito,
Antonin Scalia and Clarence Thomas, dissented.
Thomas, writing for the dissenters, said the link between the fraud claims and
smokers' health is unmistakable.
But he also said: ''The alleged misrepresentation here -- that 'light' and
'low-tar' cigarettes are not as healthy as advertised -- is actionable only
because of the effect that smoking light and low-tar cigarettes had on
respondents' health.''
Three Maine residents sued Altria Group Inc. and its Philip Morris USA Inc.
subsidiary under the state's law against unfair marketing practices. The
class-action claim represents all smokers of Marlboro Lights or Cambridge Lights
cigarettes, both made by Philip Morris.
The lawsuit argues that the company knew for decades that smokers of light
cigarettes compensate for the lower levels of tar and nicotine by taking longer
puffs and compensating in other ways.
A federal district court threw out the lawsuit, but the 1st U.S. Circuit Court
of Appeals said it could go forward.
The case is Altria Group Inc. v. Good, 07-562.
Suits Over ‘Light’ Cigarettes Allowed, NYT, 15.12.2008,
http://www.nytimes.com/aponline/2008/12/15/washington/AP-Scotus-Cigarette-Suit.html?hp
Op-Ed Contributor
Inhaling Fear
December 12, 2008
The New York Times
By MARTIN LINDSTROM
Sydney, Australia
TEN years ago, in settling the largest civil lawsuit in American history, Big
Tobacco agreed to pay the 50 states $246 billion, which they’ve used in part to
finance efforts to prevent smoking. The percentage of American adults who smoke
has fallen since then to just over 20 percent from nearly 30 percent, but
smoking is still the No. 1 preventable cause of death in the United States, and
smoking-related health care costs more than $167 billion a year.
To reduce this cost, the incoming Obama administration should abandon one
antismoking strategy that isn’t working.
A key component of the Food and Drug Administration’s approach to smoking
prevention is to warn about health dangers: Smoking causes fatal lung cancer;
smoking causes emphysema; smoking while pregnant causes birth defects. Compared
with warnings issued by other nations, these statements are low-key. From Canada
to Thailand, Australia to Brazil, warnings on cigarette packs include vivid
images of lung tumors, limbs turned gangrenous by peripheral vascular disease
and open sores and deteriorating teeth caused by mouth and throat cancers. In
October, Britain became the first European country to require similar gruesome
images on packaging.
But such warnings don’t work. Worldwide, people continue to inhale 5.7 trillion
cigarettes annually — a figure that doesn’t even take into account duty-free or
black-market cigarettes. According to World Bank projections, the number of
smokers is expected to reach 1.6 billion by 2025, from the current 1.3 billion.
A brain-imaging experiment I conducted in 2006 explains why antismoking scare
tactics have been so futile. I examined people’s brain activity as they reacted
to cigarette warning labels by using functional magnetic resonance imaging, a
scanning technique that can show how much oxygen and glucose a particular area
of the brain uses while it works, allowing us to observe which specific regions
are active at any given time.
We tested 32 people (from Britain, China, Germany, Japan and the United States),
some of whom were social smokers and some of whom were two-pack-a-day addicts.
Most of these subjects reported that cigarette warning labels reduced their
craving for a cigarette, but their brains told us a different story.
Each subject lay in the scanner for about an hour while we projected on a small
screen a series of cigarette package labels from various countries — including
statements like “smoking kills” and “smoking causes fatal lung cancers.” We
found that the warnings prompted no blood flow to the amygdala, the part of the
brain that registers alarm, or to the part of the cortex that would be involved
in any effort to register disapproval.
To the contrary, the warning labels backfired: they stimulated the nucleus
accumbens, sometimes called the “craving spot,” which lights up on f.M.R.I.
whenever a person craves something, whether it’s alcohol, drugs, tobacco or
gambling.
Further investigation is needed, but our study has already revealed an
unintended consequence of antismoking health warnings. They appear to work
mainly as a marketing tool to keep smokers smoking.
Barack Obama has said he’s been using nicotine gum to fight his own cigarette
habit. His new administration can help other smokers quit, too, by eliminating
the government scare tactics that only increase people’s craving.
Martin Lindstrom is the author of “Buyology: Truth and Lies About Why We Buy.”
Inhaling Fear, NYT,
12.12.2008,
http://www.nytimes.com/2008/12/12/opinion/12lindstrom.html
Uninsured Put a Strain on Hospitals
December 9, 2008
The New York Times
By REED ABELSON
As increasing numbers of the unemployed and uninsured turn to
the nation’s emergency rooms as a medical last resort, doctors warn that the
centers — many already overburdened — could have even more trouble handling the
heart attacks, broken bones and other traumas that define their core mission.
Even before the recession became evident, many emergency rooms around the
country were already overcrowded, with dangerously long waits for some patients
and the frequent need to redirect ambulances to other hospitals.
“We have no capacity now,” said Dr. Angela F. Gardner, the president-elect of
the American College of Emergency Physicians, which represents 27,000 emergency
doctors. “There’s no way we have room for any more people to come to the table.”
In a report to be released Tuesday, her group warns that the nation’s system of
emergency rooms is in “serious condition.” Dr. Gardner argues that any public
discussion of overhauling the current health system must include the nation’s
emergency departments.
The number of patients coming to emergency departments has been steadily
increasing. Helping push up that volume have been the growing ranks of the
uninsured, because emergency rooms are legally obliged to see all patients who
enter their doors, regardless of their ability to pay. But even insured patients
who have no quick access to regular doctors are also showing up — among them
older people, who represent the fastest growing population of emergency room
visitors.
So far, there are no firm figures on the recent influx. But even two years ago,
when a government survey found that the annual volume of visits to emergency
departments had reached 120 million — a third higher than a decade earlier —
doctors considered many emergency rooms overburdened.
Now the recession, whose full impact is yet to be seen, threatens to make
conditions even worse, emergency doctors say. Hospitals are absorbing increasing
amounts in unpaid medical bills, and some are already experiencing much higher
numbers of patients without insurance.
For example, Denver Health, a public hospital system, had a 19 percent increase
in emergency visits by uninsured patients in November — to 3,325, up from 2,792
a year earlier.
“Virtually every time I work a nine-hour shift, I encounter a couple of patients
who have never been here before because they’ve just lost their insurance,” said
Dr. Vincent J. Markovchick, the director of the hospital’s emergency medical
services.
They include patients like Matthew Armijo, 29, who was laid off from his client
services job at a technology company in August and could continue his health
insurance only through October. He showed up at Denver Health’s urgent care
center, a part of the emergency department, suffering from increasing abdominal
pain. Mr. Armijo said he went there because he would not have to pay anything.
Denver Health expects the amount of care it delivers for which it will never be
paid to grow to more than $300 million this year, compared with $276 million in
2007.
Some patients are people who have delayed seeking medical care as long as they
can, like those who arrive during an asthma attack after deferring treatment.
“I am definitely seeing patients coming in presenting worse in their illness
because they are further along,” said Dr. Katherine A. Bakes, the director of
the program’s emergency services for children.
Other doctors around the country also report treating people who seem to have no
other option. One emergency room doctor in Iowa, Dr. Thomas E. Benzoni, said he
recently saw a mother come in with her two children for what he thought was
routine care. When he asked her why she had not gone to her family doctor, she
said she did not have health insurance.
“I don’t know what else she was supposed to do,” Dr. Benzoni said.
The increase is not affecting all emergency rooms. Some emergency physicians, in
fact, said there had actually been a recent decline in visits. A report by the
American Hospital Association for July, August and September found a slight
overall decrease in hospital traffic, including emergency visits, as some people
apparently sought to avoid spending money on anything they did not deem
absolutely essential.
But as the recession continues, many officials of the college of emergency
doctors predict it is only a matter of time until the rising number of uninsured
and the delays in getting primary care create a crisis.
“I think we’re seeing the tip,” said Dr. Nicholas J. Jouriles, the group’s
current president. Patients, he said, will have no choice but to come to the
emergency department when they have no money or insurance. “They will get turned
away elsewhere,” he said.
One of the doctors’ major concerns is the long waits by patients requiring a
hospital bed. The doctors group, surveying its members last year, learned of at
least 200 deaths related to the practice of “boarding” — in which patients on
stretchers line the corridors until they can be moved into a bed.
“Crowding is a national public health problem,” said Dr. Jesse M. Pines, an
emergency physician in Philadelphia.
Patients forced to wait for hours on end for a bed clearly suffer.
“It was pure hell,” recalled Robert Roth, whose 90-year-old mother, Kato, last
year spent 36 hours at the emergency department of a Queens hospital, near her
home in Jackson Heights, waiting for a room after going to the emergency room in
the middle of the night. Mrs. Roth, who had a recent series of falls, said she
had been hearing music in her ears, and both her son and the doctor he called
were worried about a possible stroke.
After the first five hours of waiting, she became increasingly disoriented and
delusional. Mr. Roth was unable to stay with her during the entire wait. After
he left and returned, he said, the hospital staff told him they had no idea
where she was. She turned up in an empty room off the emergency department, and
her physical and mental condition had clearly deteriorated, Mr. Roth said. She
believed that she had been kidnapped.
When she had to go several weeks later to another emergency department in
Manhattan, she endured a 20-hour wait for a room, again becoming disoriented
after several hours, forcing her to be sedated.
The emergency staffs “just seemed overwhelmed, overwhelmed,” said Mr. Roth, who
wondered why emergency departments could not handle the elderly in a special
fashion.
Dr. Ann S. O’Malley is a physician and senior researcher for the Center for
Studying Health System Change, a nonprofit group in Washington that has studied
emergency services in different communities. While some hospitals have taken
steps to reduce crowding and move patients more efficiently from the emergency
department into rooms, Dr. O’Malley said, others have responded by expanding
their facilities — attracting more patients.
“Emergency departments,” she said, “are a kind of barometer of the general
health of the rest of the system.”
Dr. Eric J. Lavonas, an emergency physician in Denver, said: “The nation’s
emergency rooms are the end of the line. We will strain and stretch and bulge
under the weight.”
Dr. Gardner, of the emergency doctors’ group, said the question now is whether
the emergency room safety net will break — how often people with heart attacks
will not be able to get care in time to be saved. Her group’s report, she said,
is meant to alert people to the precarious nature of the system.
“What they don’t understand,” she said, “is that the system is fundamentally
flawed and will fail.”
Melinda Sink contributed reporting from Denver.
Uninsured Put a
Strain on Hospitals, NYT, 9.12.2008,
http://www.nytimes.com/2008/12/09/business/09emergency.html

Sharon Yacketta has had almost 20 surgeries
since a botched operation in 2004 at
University Hospital in Syracuse.
Then the errors there snowballed, a lawsuit says.
“They messed my life up,” Ms.
Yacketta said of her surgeons.
James Rajotte for The New York Times
Weak Oversight Lets Bad Hospitals Stay Open
NYT
8.12.2008
http://www.nytimes.com/2008/12/08/business/08hospital.html
The Evidence Gap
Weak
Oversight Lets Bad Hospitals Stay Open
December 8, 2008
The New York Times
By ALEX BERENSON
SYRACUSE — In March 2004, Sharon Yacketta walked into University Hospital
here for an operation to help control her incontinence.
But her doctor, Robert S. Lai, botched the procedure, causing urine to leak into
her abdomen. A month later, Dr. Lai and a second surgeon perforated her colon
during a follow-up operation at University. Four years and 20 operations later,
Ms. Yacketta has lost most of her colon and is still incontinent.
“They messed my life up,” Ms. Yacketta said of her surgeons. “I hope those
doctors rot.”
Dr. Lai, who has left University and now practices outside Chicago, acknowledged
that he and his surgical team had accidentally injured Ms. Yacketta but said he
had not been negligent.
Mistakes happen even at good hospitals, of course. But evidence shows that
University, which is owned by the State University of New York system, is not a
good hospital. In fact, in late 2006 a state commission recommended that it be
scaled back and merged with another hospital.
The state’s inability to follow through on that plan for University provides a
stark example of how hard it can be — not just in New York, but around the
nation — to close or shrink hospitals, even when there is evidence they are
providing costly and below-average care.
Certainly the evidence against University Hospital was strong. In 2006, patients
at University were three times as likely to develop infections stemming from
hospitals as were patients at the average New York hospital. HealthGrades, a
company that rates hospitals using data from Medicare, ranks University among
the least safe hospitals in the United States — although the hospital’s
executives strongly dispute that assertion. University, meanwhile, is expensive
to run.
Yet, today, University remains under state ownership. And far from shrinking,
University is expanding.
Unlike some other nations, including France, the United States has no federal
agency charged with hospital oversight. Instead, it relies on a patchwork of
state health departments and a nonprofit group called the Joint Commission that
sets basic quality standards for the nation. Hospitals are rarely closed or hit
with significant financial penalties for hurting patients.
One of the reasons is that even troubled hospitals are major employers, and
communities generally rally behind them when they face the threat of cuts, as
Syracuse did for University.
“We haven’t been forthright about the dirty little secret, the huge variation of
quality and safety in the system,” said Arthur Aaron Levin, director of the
Center for Medical Consumers, a nonprofit patient advocacy group. Nearly a
decade after the Institute of Medicine report, preventable errors remain
shockingly common, said Mr. Levin, who was a member of the commission that wrote
the report.
“It’s nine years later, and we can’t even tell you if it’s better,” Mr. Levin
said. “How is that permissible?”
Any effort to maintain national standards is left largely to Medicare and the
Joint Commission, a nonprofit group based in Oakbrook Terrace, Ill., which along
with state health departments certifies that hospitals are operating safely.
But the commission lacks the heft and enforcement powers of a federal regulator.
With fewer than 1,000 employees, it accredits and sets patient safety goals for
17,000 hospitals, nursing homes and assisted-living providers nationally. A
typical survey lasts less than a week and involves fewer than a half-dozen
examiners, said Dr. Mark R. Chassin, the president of the Joint Commission.
Hospitals account for the largest single slice of the nation’s medical spending,
31 percent, or about $650 billion in 2007, according to Medicare. Despite that
enormous bill, hospital care is uneven, and often deadly. In 1999, a report from
the Institute of Medicine found that hospital errors caused as many as 98,000
deaths a year in the United States.
Medicare is pressing for quality improvements, using as leverage the $155
billion it spends on hospital care annually. But Herb Kuhn, deputy administrator
of the Centers for Medicare and Medicaid Services, said hospitals would not make
patient safety their top priority until Medicare changed its reimbursement
system.
At present, Medicare pays the same amount to a hospital for treating a patient,
whether that patient lives or dies — even if the hospital made a preventable
error that caused the patient’s death. On Oct. 1, Medicare began a project to
end payments for a handful of “hospital-acquired conditions,” Medicare-speak for
illnesses caused by preventable errors. But the program is scheduled to reduce
reimbursement by only $21 million in 2009, not enough to make a major
difference, Mr. Kuhn said.
“We’ve got to get our payment systems changed,” he said.
States’ Efforts
While Medicare experiments, states are making their own halting efforts to
improve quality while lowering costs. Among the first was New York, which in
April 2005 created an 18-member panel to make systematic recommendations about
which hospitals and nursing homes should be closed statewide.
The need for change is acute in New York, which has among the most dysfunctional
and expensive health-care systems in the nation. In 2004, New Yorkers and their
insurers spent an average of $6,535 for each patient on health care, 24 percent
more than the national average. Yet New Yorkers are more likely to die from
chronic disease than people in any other state.
The legislation that created the panel, generally called the Berger Commission,
after its chairman, Stephen Berger, provided that its recommendations would
become law unless lawmakers overruled them.
But the legislation also provided that the state Health Department, not the
commission itself, would enforce the commission’s recommendations. That loophole
would eventually prove crucial.
On Nov. 30, 2006, after studying the state’s health-care system for almost two
years, the commission announced that nine hospitals should close and 50 others
should shrink or merge. Among the commission’s recommendations was that
University Hospital be joined with Crouse Hospital, its neighbor in Syracuse,
and that the new hospital have fewer than 600 beds, compared with the 366 beds
at University and 576 beds at Crouse, a private nonprofit hospital.
Both hospitals had problems. In 2006, patients at University had a 1-in-37
chance of suffering postoperative blood infections, compared with a 1-in-65
chance statewide, according to the Niagara Health Quality Consortium, a
nonprofit group that analyzes hospital billing records.
They had an 8.6 percent chance of dying from pneumonia, compared with a 5.5
percent chance statewide. Like HealthGrades, Niagara tries to adjust the data so
that hospitals are not penalized if the patients they treat are sicker to begin
with than those that the average hospital treats.
Crouse, for its part, had filed for bankruptcy protection in 2001 and was
running at 50 percent occupancy. Of all the commission’s recommendations,
merging University and Crouse “was the most obvious,” Mr. Berger, an investment
banker, said in a recent interview.
But University and Crouse disagreed. Days after the commission released its
report, Dr. David R. Smith, the president of Upstate Medical University, the
state-run medical school that owns University Hospital, began lobbying Eliot
Spitzer, then the governor, and Dr. Richard Daines, the state health
commissioner, to undo the recommendation.
“We’re a university, not just a hospital,” said Dr. Smith, who took over Upstate
in September 2006.
Dr. Smith and other officials at University say that the patient safety
statistics are misleading because they do not fully capture the fact that the
hospital treats very sick patients.
Dr. David Duggan, an associate dean at Upstate Medical, said that other surveys
show that University Hospital’s patient safety record is generally on par with
other hospitals. “There are some areas where I think we are above average,” Dr.
Duggan said, “and other areas where I think we need to work.”
In his battle to keep University independent of Crouse, Dr. Smith had a powerful
ally: the hospital’s unions. Most hospital employees in New York, including
those at Crouse, are represented by Local 1199. But those at University are
represented by state employees’ unions, which have richer contracts than 1199.
In 2007, University Hospital received a state subsidy of $42.2 million, about
$2,500 for each patient it admitted, to make up the difference. Not
surprisingly, University unions paid for television advertisements, lobbied
lawmakers and filed a lawsuit to overturn the recommendations.
Within Syracuse, University also had support. The medical school and hospital
are by far the largest employer in the city. “They employ people at decent
jobs,” said James Tallon, the president of the United Hospital Fund, a nonprofit
group that studies health care in New York State. “And the money comes from
Washington — money comes from elsewhere.”
By spring 2007, the state Health Department backed off the plan to join
University and Crouse, saying both could remain open and independent.
But Mr. Berger, whose commission had no authority after it filed its report in
late 2006, says the public would be better off if the state had followed its
recommendation by folding University into Crouse.
“The place that I’m most unhappy about,” he said, “is Syracuse.”
The Errors Snowball
Sharon Yacketta, 56, has not had an easy life: four brief marriages, three
children given up for adoption, six months in jail for welfare fraud. She lives
in a two-room apartment near downtown Syracuse, with dingy gray carpets and a
hulking black television.
On March 12, 2004, she entered University Hospital for an operation by Dr. Lai
to relieve her incontinence. But during the surgery, a suture punctured her
right ureter — the duct connecting the kidney to the bladder — and urine began
leaking into her abdomen, according to a lawsuit she has filed against
University that takes its details directly from her medical records.
Then the errors snowballed, according to the complaint, which lays out in flatly
clinical language three years of suffering.
Ms. Yacketta suffered near-fatal infections, endured severe pain and watched in
horror as urine and stool leaked from her body. Since the first surgery, she has
had at least 19 operations. In October 2005, she moved to St. Joseph’s Hospital,
which by many measures is the highest-rated hospital in Syracuse.
Since then, she has been under the care of Dr. B. Sivikumar, director of St.
Joseph’s surgical intensive care unit. Dr. Sivikumar said that Ms. Yacketta’s
continuing problems were very likely caused by the initial operations at
University.
After examining Ms. Yacketta’s claims, Dr. Jonathan Fine, a retired internist
and founder of At Your Side, a nonprofit group that trains volunteers as bedside
advocates for patients, said University had repeatedly made preventable errors
in her care.
“This case alone merits, from ground up, a total revamping of the procedures
that are in place in that hospital, and the culture of the hospital,” Dr. Fine
said.
Dr. Duggan said he could not comment specifically on Ms. Yacketta’s suit but
cautioned against reading too much into any one case. “We are not going to be
able to prevent every problem from occurring,” he said.
Other lawsuits, and reports from the state Health Department, also point to
problems at University. A 2005 state report refers to a case of surgery on an
infant in which “generally accepted standards of professional care were not
consistently provided,” leading the infant to be discharged prematurely and
return in less than 48 hours with kidney failure.
Another report, after a surgery in December 2006 in which doctors operated on
the wrong part of the body, criticizes the hospital for failing to make changes
promised after another “wrong-site surgery” two years before.
Dr. Smith said he had made patient safety a priority for University. “It is a
major focus of this institution,” he said.
But without faster and more accurate data gathering, no one outside University —
or any other hospital — can know whether it is doing a good job, or penalize it
if it is not, said Dr. Donald Berwick, the president of the Institute for
Healthcare Improvement, a national nonprofit group trying to reduce hospital
mistakes.
“We need to act with more speed and diligence to stop practice where it’s
actively harmful,” Dr. Berwick said. “Let the needs of patients come first, not
the needs of a hospital.”
Weak Oversight Lets Bad
Hospitals Stay Open, NYT, 8.12.2008,
http://www.nytimes.com/2008/12/08/business/08hospital.html?hp
Warning Given
on Use of 4 Popular Asthma Drugs,
but Debate
Remains
December 6, 2008
The New York Times
By GARDINER HARRIS
WASHINGTON — Two federal drug officials have concluded that asthma sufferers
risk death if they continue to use four hugely popular asthma drugs — Advair,
Symbicort, Serevent and Foradil. But the officials’ views are not universally
shared within the government.
The two officials, who work in the safety division of the Food and Drug
Administration, wrote in an assessment on the agency’s Web site on Friday that
asthma sufferers of all ages should no longer take the medicines. A third
drug-safety official concluded that Advair and Symbicort could be used by adults
but that all four drugs should no longer be used by people age 17 and under.
Dr. Badrul A. Chowdhury, director of the division of pulmonary and allergy
products at the agency, cautioned in his own assessment that the risk of death
associated with the drugs was small and that banning their use “would be an
extreme approach” that could lead asthmatics to rely on other risky medications.
Once unheard of, public disagreements among agency experts have occurred on
occasion in recent years. The agency is convening a committee of experts on
Wednesday and Thursday to sort out the disagreement, which has divided not only
the F.D.A. but also clinicians and experts for more than a decade.
Sudden deaths among asthmatics still clutching their inhalers have fed the
debate. But trying to determine whether the deaths were caused by patients’
breathing problems or the inhalers has proved difficult.
The stakes for drug makers are high. Advair sales last year were $6.9 billion
and may approach $8 billion this year, making the medication GlaxoSmithKline’s
biggest seller and one of the biggest-selling drugs in the world. Glaxo also
sells Serevent, which had $538 million in sales last year. Symbicort is made by
AstraZeneca and Foradil by Novartis.
Whatever the committee’s decision, the drugs will almost certainly remain on the
market because even the agency’s drug-safety officials concluded that they were
useful in patients suffering from chronic obstructive pulmonary disease, nearly
all of whom are elderly.
Dr. Katharine Knobil, global clinical vice president for Glaxo, dismissed the
conclusions of the agency’s drug-safety division as “not supported by their own
data.” Dr. Knobil said that Advair was safe and that Serevent was safe when used
with a steroid.
Michele Meeker, a spokeswoman for AstraZeneca, said that the F.D.A.’s safety
division improperly excluded most studies of Symbicort in its analysis, and that
a review of all of the information shows that the drug does not increase the
risks of death or hospitalization.
Dr. Daniel Frattarelli, a Detroit pediatrician and member of the American
Academy of Pediatrics’s committee on drugs, said that he was treating children
with Advair and that his committee had recently discussed the safety of the
medicines.
“Most of us felt these were pretty good drugs,” Dr. Frattarelli said. “I’m
really looking forward to hearing what the F.D.A. committee decides.”
About 9 percent of Advair’s prescriptions go to those age 17 and under,
according to Glaxo. Ms. Meeker could not provide similar figures for Symbicort.
In 1994, Serevent was approved for sale, and the F.D.A. began receiving reports
of deaths. A letter to the New England Journal of Medicine described two elderly
patients who died holding Serevent inhalers. Glaxo warned patients that the
medicine, unlike albuterol, does not work instantly and should not be used
during an attack.
In 1996, Glaxo began a study of Serevent’s safety, but the company refused for
years to report the results publicly. In 2001, the company introduced Advair,
whose sales quickly cannibalized those of Serevent and then far surpassed them.
Finally in 2003, Glaxo reported the results of its Serevent study, which showed
that those given the medicine were more likely to die than those given placebo
inhalers. Glaxo said problems with the trial made its results impossible to
interpret.
Asthma is caused when airways within the lungs spasm and swell, restricting the
supply of oxygen. The two primary treatments are steroids, which reduce
swelling, and beta agonists, which treat spasms. Rescue inhalers usually contain
albuterol, which is a beta agonist with limited duration. Serevent and Foradil
are both beta agonists but have a longer duration than albuterol and were
intended to be taken daily to prevent attacks.
Advair contains Serevent and a steroid. Symbicort, introduced last year,
contains Foradil and a steroid. In the first nine months of this year, Symbicort
had $209 million in sales.
The problem with albuterol is that it seems to make patients’ lungs more
vulnerable to severe attacks, which is why asthmatics are advised to use their
rescue inhalers only when needed. The long-acting beta agonists may have the
same risks.
But drug makers say this risk disappears when long-acting beta agonists are
paired with steroids. The labels that accompany Serevent and Foradil instruct
doctors to pair the medicines with an inhaled steroid.
Warning Given on Use of
4 Popular Asthma Drugs, but Debate Remains, NYT, 7.12.2008,
http://www.nytimes.com/2008/12/06/health/policy/06allergy.html?em
When a Job Disappears, So Does the Health Care
December 7, 2008
The New York Times
By ROBERT PEAR
ASHLAND, Ohio — As jobless numbers reach levels not seen in 25 years, another
crisis is unfolding for millions of people who lost their health insurance along
with their jobs, joining the ranks of the uninsured.
The crisis is on display here. Starla D. Darling, 27, was pregnant when she
learned that her insurance coverage was about to end. She rushed to the
hospital, took a medication to induce labor and then had an emergency Caesarean
section, in the hope that her Blue Cross and Blue Shield plan would pay for the
delivery.
Wendy R. Carter, 41, who recently lost her job and her health benefits, is
struggling to pay $12,942 in bills for a partial hysterectomy at a local
hospital. Her daughter, Betsy A. Carter, 19, has pain in her lower right jaw,
where a wisdom tooth is growing in. But she has not seen a dentist because she
has no health insurance.
Ms. Darling and Wendy Carter are among 275 people who worked at an Archway
cookie factory here in north central Ohio. The company provided excellent health
benefits. But the plant shut down abruptly this fall, leaving workers without
coverage, like millions of people battered by the worst economic crisis since
the Depression.
About 10.3 million Americans were unemployed in November, according to the
Bureau of Labor Statistics. The number of unemployed has increased by 2.8
million, or 36 percent, since January of this year, and by 4.3 million, or 71
percent, since January 2001.
Most people are covered through the workplace, so when they lose their jobs,
they lose their health benefits. On average, for each jobless worker who has
lost insurance, at least one child or spouse covered under the same policy has
also lost protection, public health experts said.
Expanding access to health insurance, with federal subsidies, was a priority for
President-elect Barack Obama and the new Democratic Congress. The increase in
the ranks of the uninsured, including middle-class families with strong ties to
the work force, adds urgency to their efforts.
“This shows why — no matter how bad the condition of the economy — we can’t
delay pursuing comprehensive health care,” said Senator Sherrod Brown, Democrat
of Ohio. “There are too many victims who are innocent of anything but working at
the wrong place at the wrong time.”
Some parts of the federal safety net are more responsive to economic distress.
The number of people on food stamps set a record in September, with 31.6 million
people receiving benefits, up by two million in one month.
Nearly 4.4 million people are receiving unemployment insurance benefits, an
increased of 60 percent in the past year. But more than half of unemployed
workers are not getting help because they do not qualify or have exhausted their
benefits.
About 1.7 million families receive cash under the main federal-state welfare
program, little changed from a year earlier. Welfare serves about 4 of 10
eligible families and fewer than one in four poor children.
In a letter dated Oct. 3, Archway told workers that their jobs would be
eliminated, and their insurance terminated on Oct. 6, because of “unforeseeable
business circumstances.” The company, owned by a private equity firm based in
Greenwich, Conn., filed a petition for relief under Chapter 11 of the Bankruptcy
Code.
Archway workers typically made $13 to $20 an hour. To save money in a tough
economy, they are canceling appointments with doctors and dentists, putting off
surgery, and going without prescription medicines for themselves and their
children.
Archway cited “the challenging economic environment” as a reason for closing.
“We have been operating at a loss due largely to the significant increases in
raw material costs, such as flour, butter, sugar and dairy, and the record high
fuel costs across the country,” the company said. At this time of year, the
Archway plant is usually bustling as employees work overtime to make Christmas
cookies. This year the plant is silent. The aromas of cinnamon and licorice are
missing. More than 40 trailers sit in the parking lot with nothing to haul.
In the weeks before it filed for bankruptcy protection, Archway apparently fell
behind in paying for its employee health plan. In its bankruptcy filing, Archway
said it owed more than $700,000 to Blue Cross and Blue Shield of Illinois, one
of its largest creditors.
Richard D. Jackson, 53, was an oven operator at the bakery for 30 years. He and
his two daughters often used the Archway health plan to pay for doctor’s visits,
imaging, surgery and medicines. Now that he has no insurance, Mr. Jackson takes
his Effexor antidepressant pills every other day, rather than daily, as
prescribed.
Another former Archway employee, Jeffrey D. Austen, 50, said he had canceled
shoulder surgery scheduled for Oct. 13 at the Cleveland Clinic because he had no
way to pay for it.
“I had already lined up an orthopedic surgeon and an anesthesiologist,” Mr.
Austen said.
In mid-October, Janet M. Esbenshade, 37, who had been a packer at the Archway
plant, began to notice that her vision was blurred. “My eyes were burning,
itching and watery,” she said. “Pus was oozing out. If I had had insurance, I
would have gone to an eye doctor right away.”
She waited two weeks. The infection became worse. She went to the hospital on
Oct. 26. Doctors found that she had keratitis, a painful condition that she may
have picked up from an old pair of contact lenses. They prescribed antibiotics,
which have cleared up the infection.
Ms. Esbenshade has two daughters, ages 6 and 10, with asthma. She has explained
to them why “we are not Christmas shopping this year — unless, by some miracle,
mommy goes back to work and gets a paycheck.”
She said she had told the girls, “I would rather you stay out of the hospital
and take your medication than buy you a little toy right now because I think
your health is more important.”
In some cases, people who are laid off can maintain their group health benefits
under a federal law, the Consolidated Omnibus Budget Reconciliation Act of 1986,
known as Cobra. But that is not an option for former Archway employees because
their group health plan no longer exists. And they generally cannot afford to
buy insurance on their own.
Wendy Carter’s case is typical. She receives $956 a month in unemployment
benefits. Her monthly expenses include her share of the rent ($300), car
payments ($300), auto insurance ($75), utilities ($220) and food ($260). That
leaves nothing for health insurance.
Ms. Darling, who was pregnant when her insurance ran out, worked at Archway for
eight years, and her father, Franklin J. Phillips, worked there for 24 years.
“When I heard that I was losing my insurance,” she said, “I was scared. I
remember that the bill for my son’s delivery in 2005 was about $9,000, and I
knew I would never be able to pay that by myself.”
So Ms. Darling asked her midwife to induce labor two days before her health
insurance expired.
“I was determined that we were getting this baby out, and it was going to be
paid for,” said Ms. Darling, who was interviewed at her home here as she cradled
the infant in her arms.
As it turned out, the insurance company denied her claim, leaving Ms. Darling
with more than $17,000 in medical bills.
The latest official estimate of the number of uninsured, from the Census Bureau,
is for 2007, when the economy was in better condition. In that year, the bureau
says, 45.7 million people, accounting for 15.3 percent of the population, were
uninsured.
M. Harvey Brenner, a professor of public health at the University of North Texas
and Johns Hopkins University, said that three decades of research had shown a
correlation between the condition of the economy and human health, including
life expectancy.
“In recessions, with declines in national income and increases in unemployment,
you often see increases in mortality from heart disease, cancer, psychiatric
illnesses and other conditions,” Mr. Brenner said.
The recession is also taking a toll on hospitals.
“We have seen a significant increase in patients seeking assistance paying their
bills,” said Erin M. Al-Mehairi, a spokeswoman for Samaritan Hospital in
Ashland. “We’ve had a 40 percent increase in charity care write-offs this year
over the 2007 level of $2.7 million.”
In addition, people are using the hospital less. “We’ve seen a huge decrease in
M.R.I.’s, CAT scans, stress tests, cardiac catheterization tests, knee and hip
replacements and other elective surgery,” Ms. Al-Mehairi said.
When a Job Disappears,
So Does the Health Care, NYT, 7.12.2008,
http://www.nytimes.com/2008/12/07/us/07uninsured.html?hp
H. M., an Unforgettable Amnesiac, Dies at 82
December 5, 2008
The New York Times
By BENEDICT CAREY
He knew his name. That much he could remember.
He knew that his father’s family came from Thibodaux, La., and his mother was
from Ireland, and he knew about the 1929 stock market crash and World War II and
life in the 1940s.
But he could remember almost nothing after that.
In 1953, he underwent an experimental brain operation in Hartford to correct a
seizure disorder, only to emerge from it fundamentally and irreparably changed.
He developed a syndrome neurologists call profound amnesia. He had lost the
ability to form new memories.
For the next 55 years, each time he met a friend, each time he ate a meal, each
time he walked in the woods, it was as if for the first time.
And for those five decades, he was recognized as the most important patient in
the history of brain science. As a participant in hundreds of studies, he helped
scientists understand the biology of learning, memory and physical dexterity, as
well as the fragile nature of human identity.
On Tuesday evening at 5:05, Henry Gustav Molaison — known worldwide only as H.
M., to protect his privacy — died of respiratory failure at a nursing home in
Windsor Locks, Conn. His death was confirmed by Suzanne Corkin, a neuroscientist
at the Massachusetts Institute of Technology, who had worked closely with him
for decades. Henry Molaison was 82.
From the age of 27, when he embarked on a life as an object of intensive study,
he lived with his parents, then with a relative and finally in an institution.
His amnesia did not damage his intellect or radically change his personality.
But he could not hold a job and lived, more so than any mystic, in the moment.
“Say it however you want,” said Dr. Thomas Carew, a neuroscientist at the
University of California, Irvine, and president of the Society for Neuroscience.
“What H. M. lost, we now know, was a critical part of his identity.”
At a time when neuroscience is growing exponentially, when students and money
are pouring into laboratories around the world and researchers are mounting
large-scale studies with powerful brain-imaging technology, it is easy to forget
how rudimentary neuroscience was in the middle of the 20th century.
When Mr. Molaison, at 9 years old, banged his head hard after being hit by a
bicycle rider in his neighborhood near Hartford, scientists had no way to see
inside his brain. They had no rigorous understanding of how complex functions
like memory or learning functioned biologically. They could not explain why the
boy had developed severe seizures after the accident, or even whether the blow
to the head had anything do to with it.
Eighteen years after that bicycle accident, Mr. Molaison arrived at the office
of Dr. William Beecher Scoville, a neurosurgeon at Hartford Hospital. Mr.
Molaison was blacking out frequently, had devastating convulsions and could no
longer repair motors to earn a living.
After exhausting other treatments, Dr. Scoville decided to surgically remove two
finger-shaped slivers of tissue from Mr. Molaison’s brain. The seizures abated,
but the procedure — especially cutting into the hippocampus, an area deep in the
brain, about level with the ears — left the patient radically changed.
Alarmed, Dr. Scoville consulted with a leading surgeon in Montreal, Dr. Wilder
Penfield of McGill University, who with Dr. Brenda Milner, a psychologist, had
reported on two other patients’ memory deficits.
Soon Dr. Milner began taking the night train down from Canada to visit Mr.
Molaison in Hartford, giving him a variety of memory tests. It was a
collaboration that would forever alter scientists’ understanding of learning and
memory.
“He was a very gracious man, very patient, always willing to try these tasks I
would give him,” Dr. Milner, a professor of cognitive neuroscience at the
Montreal Neurological Institute and McGill University, said in a recent
interview. “And yet every time I walked in the room, it was like we’d never
met.”
At the time, many scientists believed that memory was widely distributed
throughout the brain and not dependent on any one neural organ or region. Brain
lesions, either from surgery or accidents, altered people’s memory in ways that
were not easily predictable. Even as Dr. Milner published her results, many
researchers attributed H. M.’s deficits to other factors, like general trauma
from his seizures or some unrecognized damage.
“It was hard for people to believe that it was all due” to the excisions from
the surgery, Dr. Milner said.
That began to change in 1962, when Dr. Milner presented a landmark study in
which she and H. M. demonstrated that a part of his memory was fully intact. In
a series of trials, she had Mr. Molaison try to trace a line between two
outlines of a five-point star, one inside the other, while watching his hand and
the star in a mirror. The task is difficult for anyone to master at first.
Every time H. M. performed the task, it struck him as an entirely new
experience. He had no memory of doing it before. Yet with practice he became
proficient. “At one point he said to me, after many of these trials, ‘Huh, this
was easier than I thought it would be,’ ” Dr. Milner said.
The implications were enormous. Scientists saw that there were at least two
systems in the brain for creating new memories. One, known as declarative
memory, records names, faces and new experiences and stores them until they are
consciously retrieved. This system depends on the function of medial temporal
areas, particularly an organ called the hippocampus, now the object of intense
study.
Another system, commonly known as motor learning, is subconscious and depends on
other brain systems. This explains why people can jump on a bike after years
away from one and take the thing for a ride, or why they can pick up a guitar
that they have not played in years and still remember how to strum it.
Soon “everyone wanted an amnesic to study,” Dr. Milner said, and researchers
began to map out still other dimensions of memory. They saw that H. M.’s
short-term memory was fine; he could hold thoughts in his head for about 20
seconds. It was holding onto them without the hippocampus that was impossible.
“The study of H. M. by Brenda Milner stands as one of the great milestones in
the history of modern neuroscience,” said Dr. Eric Kandel, a neuroscientist at
Columbia University. “It opened the way for the study of the two memory systems
in the brain, explicit and implicit, and provided the basis for everything that
came later — the study of human memory and its disorders.”
Living at his parents’ house, and later with a relative through the 1970s, Mr.
Molaison helped with the shopping, mowed the lawn, raked leaves and relaxed in
front of the television. He could navigate through a day attending to mundane
details — fixing a lunch, making his bed — by drawing on what he could remember
from his first 27 years.
He also somehow sensed from all the scientists, students and researchers
parading through his life that he was contributing to a larger endeavor, though
he was uncertain about the details, said Dr. Corkin, who met Mr. Molaison while
studying in Dr. Milner’s laboratory and who continued to work with him until his
death.
By the time he moved into a nursing home in 1980, at age 54, he had become known
to Dr. Corkin’s M.I.T. team in the way that Polaroid snapshots in a photo album
might sketch out a life but not reveal it whole.
H. M. could recount childhood scenes: Hiking the Mohawk Trail. A road trip with
his parents. Target shooting in the woods near his house.
“Gist memories, we call them,” Dr. Corkin said. “He had the memories, but he
couldn’t place them in time exactly; he couldn’t give you a narrative.”
He was nonetheless a self-conscious presence, as open to a good joke and as
sensitive as anyone in the room. Once, a researcher visiting with Dr. Milner and
H. M. turned to her and remarked how interesting a case this patient was.
“H. M. was standing right there,” Dr. Milner said, “and he kind of colored —
blushed, you know — and mumbled how he didn’t think he was that interesting, and
moved away.”
In the last years of his life, Mr. Molaison was, as always, open to visits from
researchers, and Dr. Corkin said she checked on his health weekly. She also
arranged for one last research program. On Tuesday, hours after Mr. Molaison’s
death, scientists worked through the night taking exhaustive M.R.I. scans of his
brain, data that will help tease apart precisely which areas of his temporal
lobes were still intact and which were damaged, and how this pattern related to
his memory.
Dr. Corkin arranged, too, to have his brain preserved for future study, in the
same spirit that Einstein’s was, as an irreplaceable artifact of scientific
history.
“He was like a family member,” said Dr. Corkin, who is at work on a book on H.
M., titled “A Lifetime Without Memory.” “You’d think it would be impossible to
have a relationship with someone who didn’t recognize you, but I did.”
In his way, Mr. Molaison did know his frequent visitor, she added: “He thought
he knew me from high school.”
Henry Gustav Molaison, born on Feb. 26, 1926, left no survivors. He left a
legacy in science that cannot be erased.
H. M., an Unforgettable
Amnesiac, Dies at 82, NYT, 5.12.2008,
http://www.nytimes.com/2008/12/05/us/05hm.html?hp
Parents Torn Over Fate of Frozen Embryos
December 4, 2008
The New York Times
By DENISE GRADY
For nearly 15 years, Kim and Walt Best have been paying about $200 a year to
keep nine embryos stored in a freezer at a fertility clinic at Duke University —
embryos that they no longer need, because they are finished having children but
that Ms. Best cannot bear to destroy, donate for research or give away to
another couple.
The embryos were created by in vitro fertilization, which gave the Bests a set
of twins, now 14 years old.
Although the couple, who live in Brentwood, Tenn., have known for years that
they wanted no more children, deciding what to do with the extra embryos has
been a dilemma. He would have them discarded; she cannot.
“There is no easy answer,” said Ms. Best, a nurse. “I can’t look at my twins and
not wonder sometimes what the other nine would be like. I will keep them frozen
for now. I will search in my heart.”
At least 400,000 embryos are frozen at clinics around the country, with more
being added every day, and many people who are done having children are finding
it harder than they had ever expected to decide the fate of those embryos.
A new survey of 1,020 fertility patients at nine clinics reveals more than a
little discontent with the most common options offered by the clinics. The
survey, in which Ms. Best took part, is being published on Thursday in the
journal Fertility and Sterility.
Among patients who wanted no more children, 53 percent did not want to donate
their embryos to other couples, mostly because they did not want someone else
bringing up their children, or did not want their own children to worry about
encountering an unknown sibling someday.
Forty-three percent did not want the embryos discarded. About 66 percent said
they would be likely to donate the embryos for research, but that option was
available at only four of the nine clinics in the survey. Twenty percent said
they were likely to keep the embryos frozen forever.
Embryos can remain viable for a decade or more if they are frozen properly but
not all of them survive when they are thawed.
Smaller numbers of patients wished for solutions that typically are not offered.
Among them were holding a small ceremony during the thawing and disposal of the
embryos, or having them placed in the woman’s body at a time in her cycle when
she would probably not become pregnant, so that they would die naturally.
The message from the survey is that patients need more information, earlier in
the in vitro process, to let them know that frozen embryos may result and that
deciding what to do with them in the future “may be difficult in ways you don’t
anticipate,” said Dr. Anne Drapkin Lyerly, the first author of the study and a
bioethicist and associate professor of obstetrics and gynecology at Duke
University.
Dr. Lyerly also said discussions about the embryos should be “revisited, and not
happen just at the time of embryo freezing, because people’s goals and their way
of thinking about embryos change as time passes and they go through infertility
treatment.”
Many couples are so desperate to have a child that when eggs are fertilized in
the clinic, they want to create as many embryos as possible, to maximize their
chances, Dr. Lyerly said. At that time, the notion that there could be too many
embryos may seem unimaginable. (In Italy, fertility clinics are not allowed to
create more embryos than can be implanted in the uterus at one time,
specifically to avoid the ethical quandary posed by frozen embryos.)
In a previous study by Dr. Lyerly, women expressed wide-ranging views about
embryos: one called them “just another laboratory specimen,” but another said a
freezer full of embryos was “like an orphanage.”
Dr. Mark V. Sauer, the director of the Center for Women’s Reproductive Care at
Columbia University Medical Center in Manhattan, said: “It’s a huge issue. And
the wife and husband may not be on the same page.”
Some people pay storage fees for years and years, Dr. Sauer said. Others stop
paying and disappear, leaving the clinic to decide whether to maintain the
embryos free or to get rid of them.
“They would rather have you pull the trigger on the embryos,” Dr. Sauer said.
“It’s like, ‘I don’t want another baby, but I don’t have it in me; I have too
much guilt to tell you what to do, to have them discarded.’ ”
A few patients have asked that extra embryos be given to them, and he
cooperates, Dr. Sauer said, adding, “I don’t know if they take them home and
bury them.”
Federal and state regulations have made it increasingly difficult for those who
want to donate to other couples, requiring that donors come back to the clinic
to be screened for infectious diseases, sometimes at their own expense, Dr.
Sauer said.
“It’s partly reflected in the attitude of the clinics,” he said, explaining that
he does not even suggest that people give embryos to other couples anymore,
whereas 10 years ago many patients did donate.
Ms. Best said her nine embryos “have the potential to become beautiful people.”
The thought of giving them up for research “conjures all sorts of horrors, from
Frankenstein to the Holocaust,” she said, adding that destroying them would be
preferable.
Her teenage daughter favors letting another couple adopt the embryos, but, Ms.
Best said, she would worry too much about “what kind of parents they were with,
what kind of life they had.”
Another survey participant, Lynnelle Fowler McDonald, a case manager for a
nonprofit social service agency in Durham, N.C., has one embryo frozen at Duke,
all that is left of three failed efforts at the fertility clinic.
Given the physical and emotional stress, and the expense of in vitro
fertilization, Ms. McDonald said she did not know whether she and her husband
could go through it again. But to get rid of that last embryo would be final; it
would mean they were giving up.
“There is still, in the back of my mind, this hope,” she said.
At the Genetics and IVF Institute in Fairfax, Va., Andrew Dorfmann, the chief
embryologist, said many patients were genuinely torn about what to do with extra
embryos, and that a few had asked to be present to say a prayer when their
embryos were thawed and destroyed.
Jacqueline Betancourt, a marketing analyst with a software company who took part
in the survey, said she and her husband donated their embryos at Duke “to
science, whatever that means.” It was important to them that the embryos were
not just going to be discarded without any use being made of them.
Ms. Betancourt, who has two sons, said: “We didn’t ask many questions. We were
just comfortable with the idea that they weren’t going to be destroyed. We
didn’t see the point in destroying something that could be useful to science, to
other people, to helping other people.”
Ms. Betancourt said she wished there had been more discussion about the extra
embryos early in the process. If she had known more, she said, she might have
considered creating fewer embryos in the first place.
Parents Torn Over Fate of Frozen Embryos, NYT,
4.12.2008,
http://www.nytimes.com/2008/12/04/us/04embryo.html?hp
Mind
Standing in Someone
Else’s Shoes, Almost for Real
December 2,
2008
The New York Times
By BENEDICT CAREY
From the
outside, psychotherapy can look like an exercise in self-absorption. In fact,
though, therapists often work to pull people out of themselves: to see their
behavior from the perspective of a loved one, for example, or to observe their
own thinking habits from a neutral distance.
Marriage counselors have couples role-play, each one taking the other spouse’s
part. Psychologists have rapists and other criminals describe their crime from
the point of view of the victim. Like novelists or moviemakers, their purpose is
to transport people, mentally, into the mind of another.
Now, neuroscientists have shown that they can make this experience physical,
creating a “body swapping” illusion that could have a profound effect on a range
of therapeutic techniques. At the annual meeting of the Society for Neuroscience
last month, Swedish researchers presented evidence that the brain, when tricked
by optical and sensory illusions, can quickly adopt any other human form, no
matter how different, as its own.
“You can see the possibilities, putting a male in a female body, young in old,
white in black and vice versa,” said Dr. Henrik Ehrsson of the Karolinska
Institute in Stockholm, who with his colleague Valeria Petkova described the
work to other scientists at the meeting. Their full study is to appear online
this week in the journal PLoS One. .
The technique is simple. A subject stands or sits opposite the scientist, as if
engaged in an interview.. Both are wearing headsets, with special goggles, the
scientist’s containing small film cameras. The goggles are rigged so the subject
sees what the scientist sees: to the right and left are the scientist’s arms,
and below is the scientist’s body.
To add a physical element, the researchers have each person squeeze the other’s
hand, as if in a handshake. Now the subject can see and “feel” the new body. In
a matter of seconds, the illusion is complete. In a series of studies, using
mannequins and stroking both bodies’ bellies simultaneously, the Karolinska
researchers have found that men and women say they not only feel they have taken
on the new body, but also unconsciously cringe when it is poked or threatened.
In previous work, neuroscientists have induced various kinds of out-of-body
experiences using similar techniques. The brain is so easily tricked, they say,
precisely because it has spent a lifetime in its own body. It builds models of
the world instantaneously, based on lived experience and using split-second
assumptions — namely, that the eyes are attached to the skull.
Therapists say the body-swapping effect is so odd that it could be risky for
anyone in real mental distress. People suffering from the delusions of
schizophrenia or the grandiose mania of bipolar disorder are not likely to
benefit from more disorientation, no matter the intent.
But those who seek help for relationship problems, in particular, often begin to
moderate their behavior only after they have worked to see the encounters in
their daily life from others’ point of view.
“This is especially true for adolescents, who are so self-involved, and also for
people who come in with anger problems and are more interested in changing
everyone else in their life than themselves,” said Kristene Doyle, director of
clinical services at the Albert Ellis Institute in New York.
One important goal of therapy in such cases, Dr. Doyle said, is to get people to
generate alternative explanations for others’ behavior — before they themselves
react.
The evidence that inhabiting another’s perspective can change behavior comes in
part from virtual-reality experiments. In these studies, researchers create
avatars that mimic a person’s every movement. After watching their “reflection”
in a virtual mirror, people mentally inhabit this avatar at some level,
regardless of its sex, race or appearance. In several studies, for instance,
researchers have shown that white people who spend time interacting virtually as
black avatars become less anxious about racial differences.
Jeremy Bailenson, director of the Virtual Human Interaction Lab at Stanford
University, and his colleague Nick Yee call this the Proteus effect, after the
Greek god who can embody many different self-representations.
In one experiment, the Stanford team found that people inhabiting physically
attractive avatars were far more socially intimate in virtual interactions than
those who had less appealing ones. The effect was subconscious: the study
participants were not aware that they were especially good-looking, or that in
virtual conversations they moved three feet closer to virtual conversation
partners and revealed more about themselves than others did. This confidence
lingered even after the experiment was over, when the virtual lookers picked
more attractive partners as matches for a date.
Similar studies have found that people agree to contribute more to retirement
accounts when they are virtually “age-morphed” to look older; and that they will
exercise more after inhabiting an avatar that works out and loses weight.
Adding a physical body-swapping element, as the Swedish team did, is likely to
amplify such changes. “It has video quality, it looks and feels more realistic
than what we can do in virtual environments, so is likely to be much more
persuasive,” Dr. Bailenson said in a telephone interview.
Perhaps too persuasive for some purposes. “It may be like the difference between
a good book, where you can project yourself into a character by filling in with
your imagination, and a movie, where the specific actor gets in the way of
identifying strongly,” he went on.
And above and beyond any therapeutic purposes, the sensation is downright
strange. In the experiments, said Dr. Ehrsson, the Swedish researcher, “even the
feeling from the squeezing hand is felt in the scientist’s hand and not in your
own; this is perhaps the strangest aspect of the experience.”
Standing in Someone Else’s Shoes, Almost for Real, NYT,
2.12.2008,
http://www.nytimes.com/2008/12/02/health/02mind.html
|