|
History > 2008 > USA > Health (I)
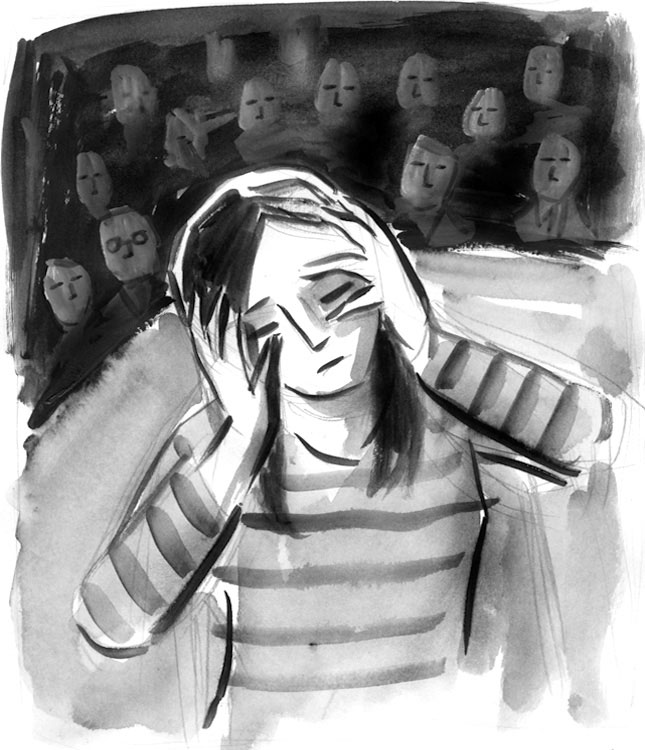
Illustration: Mark Weber
Fibromyalgia: The Pain Is Very Real
NYT
17.1.2008
https://www.nytimes.com/2008/01/17/
opinion/l17disease.html
Bush Seeks Surplus
via Medicare Cuts
January 31, 2008
The New York Times
By ROBERT PEAR
WASHINGTON — In his new budget, to be unveiled Monday,
President Bush will call for large cuts in the growth of Medicare, far exceeding
what he proposed last year, and he will again seek major savings in Medicaid,
according to administration officials and budget documents.
Over all, the 2009 budget is likely to be the first $3 trillion spending request
by a president.
Health care savings are a crucial part of Mr. Bush’s plan to put the nation on
track to achieve a budget surplus by 2012. But before then, the officials said
Wednesday, the White House anticipates higher deficits in 2008 and 2009,
reflecting the current weakness of the economy and the cost of a stimulus
package.
The president’s budget will not seek money for another full year of the wars in
Iraq and Afghanistan. Pentagon officials said the administration would request
$70 billion for the fiscal year that begins on Oct. 1. That would be enough to
continue combat operations for several months, until the next president takes
office.
Mr. Bush has repeatedly said that the costs of Medicare and Medicaid, which
dwarf spending for lawmakers’ pet projects, are unsustainable. The two health
programs account for nearly one-fourth of all federal spending, and their
combined cost — $627 billion last year — is expected to double in a decade.
Budget documents show that Mr. Bush will propose legislative changes in Medicare
to save $6 billion in the next year and $91 billion from 2009 to 2013. In his
last budget, by contrast, his legislative proposals would have saved $4 billion
in the first year and $65.6 billion over five years.
The president’s budget also takes aim at Medicaid, the insurance program for
low-income people. He would pare $1.2 billion from it next year and nearly $14
billion over five years.
Those figures do not include tens of billions of dollars that Mr. Bush wants to
save through new regulations. Such rules are not subject to approval by
Congress, but could be revised by a future administration.
Congressional Democrats often pronounce Mr. Bush’s budget dead on arrival, and
they have no reason to make unpopular cuts in this election year.
But lawmakers say they feel obliged to pass a Medicare bill in the first half of
this year, to spare doctors from a 10 percent cut in Medicare fees that would
otherwise take effect on July 1. Lawmakers say that bill could easily become a
vehicle for other changes in Medicare and Medicaid.
Most of the Medicare savings in the budget would be achieved by reducing the
annual update in federal payments to hospitals, nursing homes, hospices,
ambulances and home care agencies.
The budget would not touch payments to insurance companies for private Medicare
Advantage plans, even though many Democrats and independent experts say those
plans are overpaid.
In the next five years, the largest amount of Medicare savings, by far, would
come from hospitals: $15 billion from an across-the-board reduction in the
annual updates for inpatient care; $25 billion from special payments to
hospitals serving large numbers of poor people; and $20 billion from capital
payments for the construction of hospital buildings and the purchase of
equipment.
In addition, the president’s budget would reduce special Medicare payments to
teaching hospitals, including many in the New York area, by $23 billion over the
next five years.
To justify prior budget proposals, the White House has often cited the work of
an independent federal panel, the Medicare Payment Advisory Commission. The
panel voted this month to recommend that Medicare payments to hospitals be
increased about 3 percent in 2009, to reflect the expected increase in the cost
of goods and services hospitals use. Under the president’s budget, Medicare
payments would not keep pace with those costs in 2009 or any subsequent year.
The advisory panel found that the special Medicare payments to teaching
hospitals were excessive, as the White House contends. But it recommended a much
more modest cutback than Mr. Bush will propose.
Kenneth E. Raske, president of the Greater New York Hospital Association, said
the president’s proposals showed “great insensitivity to teaching hospitals”
across the country. The proposals “would undermine our ability to train young
doctors at a time when the nation is facing a shortage of doctors,” Mr. Raske
said.
Under the president’s budget, Medicare payment rates for nursing homes would be
frozen in 2009, and payment rates for home health agencies would be frozen at
current levels through 2013.
William A. Dombi, vice president of the National Association for Home Care and
Hospice, a trade group, said the proposal could affect many of the three million
Medicare beneficiaries who receive home health services each year.
“Under the proposal,” Mr. Dombi said, “75 percent to 80 percent of home health
agencies would be doomed. They would not be able to meet payroll. They would not
be able to operate.”
Within 15 days of sending his budget to Congress, Mr. Bush is supposed to submit
legislation to strengthen the financial condition of Medicare and to reduce its
reliance on general revenues, which include income taxes. The 2003 Medicare law
established special procedures to ensure that Congress would consider such
legislation.
House Democrats want to eliminate this requirement, saying it is a Republican
device to undermine Medicare’s status as an entitlement.
Bush Seeks Surplus
via Medicare Cuts, NYT, 31.1.2008,
http://www.nytimes.com/2008/01/31/washington/31budget.html
Lilly Considers $1 Billion Fine
to Settle Case
January 31, 2008
The New York Times
By ALEX BERENSON
Eli Lilly and federal prosecutors are discussing a settlement
of a civil and criminal investigation into the company’s marketing of the
antipsychotic drug Zyprexa that could result in Lilly’s paying more than $1
billion to federal and state governments.
If a deal is reached, the fine would be the largest ever paid by a drug company
for breaking the federal laws that govern how drug makers can promote their
medicines.
Several people involved in the investigation confirmed the settlement
discussions, which began last year and took on new urgency this month. The
people insisted on anonymity because they have not been authorized to talk about
the negotiations.
Zyprexa has serious side effects and is approved only to treat people with
schizophrenia and severe bipolar disorder. But documents from Eli Lilly show
that from 2000 to 2003 the company encouraged doctors to prescribe Zyprexa to
people with age-related dementia, as well as people with mild bipolar disorder
who had previously had a diagnosis of depression.
Although doctors can prescribe drugs for any use once they are on the market, it
is illegal for drug makers to promote their medicines for any uses not formally
approved by the Food and Drug Administration.
Lilly may also plead guilty to a misdemeanor criminal charge as part of the
agreement, the people involved with the investigation said. But the company
would be allowed to keep selling Zyprexa to Medicare and Medicaid, the
government programs that are the biggest customers of the drug.
Zyprexa is Lilly’s most profitable product and among the world’s best-selling
medicines, with 2007 sales of $4.8 billion, about half in the United States.
Lilly would neither confirm nor deny the settlement talks.
“We have been and are continuing to cooperate in state and federal
investigations related to Zyprexa, including providing a broad range of
documents and information,” Lilly said in a statement Wednesday afternoon. “As
part of that cooperation we regularly have discussions with the government.
However, we have no intention of sharing those discussions with the news media
and it would be speculative and irresponsible for anyone to do so.”
Lilly also said that it had always followed state and federal laws when
promoting Zyprexa.
The Lilly fine would be distributed among federal and state governments, which
spend about $1.5 billion on Zyprexa each year through Medicare and Medicaid.
The fine would be in addition to $1.2 billion that Lilly has already paid to
settle 30,000 lawsuits from people who claim that Zyprexa caused them to develop
diabetes or other diseases. Zyprexa can cause severe weight gain in many
patients and has been linked to diabetes by the American Diabetes Association.
Prescriptions for Zyprexa have skidded since 2003 over concerns about those side
effects. But the drug continues to be widely used, especially among severely
mentally ill patients. Many psychiatrists say that it works better than other
medicines at calming patients who are psychotic and hallucinating. About four
million Zyprexa prescriptions were written in the United States last year.
Federal prosecutors in Philadelphia are leading the settlement talks for the
government, in consultation with the Justice Department in Washington. State
attorneys general’s offices are also involved. Lawyers at Pepper Hamilton, a
firm based in Philadelphia, and Sidley Austin, a firm based in Chicago, are
negotiating for Lilly.
Nina Gussack, a lawyer at Pepper Hamilton who is representing Lilly, said she
could not comment on the case. Joseph Trautwein, an assistant United States
attorney for the Eastern District of Pennsylvania, also declined to comment.
While a settlement has not been concluded and the negotiations could collapse,
both sides want to reach an agreement, according to the people involved in the
investigation.
Besides the escalating pressure of the federal criminal inquiry, Lilly faces a
civil trial scheduled for March in Anchorage, in a lawsuit brought by the state
of Alaska to recover money the state has spent on Zyprexa prescriptions. A loss
in that lawsuit would damage Lilly’s bargaining position in the Philadelphia
talks.
While expensive for Lilly, the settlement would end a four-year federal
investigation and remove a cloud over Zyprexa. While Zyprexa prescriptions are
falling, its dollar volume of sales is rising because Lilly has raised Zyprexa’s
price about 40 percent since 2003.
Federal prosecutors have been investigating Lilly for its marketing of Zyprexa
since 2004, and state attorneys general have been doing so since 2005. The
people involved in the investigations said the inquiries gained momentum after
December 2006, when The New York Times published articles describing Lilly’s
years-long efforts to play down Zyprexa’s side effects and to promote the drug
for conditions other than schizophrenia and severe bipolar disorder — a practice
called off-label marketing.
Internal Lilly marketing documents and e-mail messages showed that Lilly wanted
to persuade doctors to prescribe Zyprexa for patients with age-related dementia
or relatively mild bipolar disorder.
In one document, an unidentified Lilly marketing executive wrote that primary
care doctors “do treat dementia” but leave schizophrenia and bipolar disorder to
psychiatrists. As a result, sales representatives should discuss dementia with
primary care doctors, according to the document, which appears to be part of a
larger marketing presentation but is not marked more specifically. Later, the
same document says that some primary care doctors “might prescribe outside of
label.”
In late 2000, Lilly began a marketing campaign called Viva Zyprexa and told
sales representatives to suggest that doctors prescribe Zyprexa to older
patients with symptoms of dementia.
The documents were under federal court seal when The Times published the
articles, and Judge Jack B. Weinstein of United States District Court in
Brooklyn rebuked The Times for publishing them.
The settlement negotiations in Philadelphia began several months ago, according
to the people involved in the investigation.
Last fall, the two sides were close to a deal in which Lilly would have paid
less than $1 billion to settle the case, which at the time consisted only of a
civil complaint.
Then Justice Department lawyers in Washington pressed for a grand jury
investigation to examine whether Lilly should be charged criminally for its
promotional activities, according to the people involved in the negotiations. A
few days ago, facing the possibility of both civil and criminal charges, Lilly
opened new discussions with the prosecutors in Philadelphia.
Lilly Considers $1
Billion Fine to Settle Case, NYT, 31.1.2008,
http://www.nytimes.com/2008/01/31/business/31drug.html?hp
F.D.A. Requiring Suicide Studies
in Drug Trials
January 24, 2008
The New York Times
By GARDINER HARRIS
After decades of inattention to the possible psychiatric side
effects of experimental medicines, the Food and Drug Administration is now
requiring drug makers to study closely whether patients become suicidal during
clinical trials.
The new rules represent one of the most profound changes of the past 16 years to
regulations governing drug development. But since the F.D.A.’s oversight of
experimental medicines is done in secret, the agency’s shift has not been
announced publicly.
The drug industry, however, is keenly aware of the change. Makers of drugs to
treat obesity, urinary incontinence, epilepsy, smoking cessation, depression and
many other conditions are being asked for the first time by the drug agency to
put a comprehensive suicide assessment into their clinical trials.
In recent months, the agency has sent letters — it would not say how many — to
drug makers requiring that they use such a scale. Merck, Sanofi-Aventis and Eli
Lilly are all using a detailed suicide assessment in clinical trials being
conducted now.
The seeds for the new federal effort were planted four years ago with the
discovery that antidepressants may cause some children and teenagers to become
suicidal. Top agency officials at first discounted the finding but commissioned
researchers from Columbia University’s department of psychiatry, led by Kelly L.
Posner, to reanalyze the drugs’ clinical trials. This work caused the drug
agency and its experts to view the risk as real.
Then it received an application for rimonabant, a much-heralded obesity drug
developed by the French drug giant, Sanofi-Aventis. As agency medical reviewers
pored over the drug’s clinical trial data, they discovered hints that it could
cause psychiatric problems, too.
Unsettled by their experience with antidepressants, agency reviewers again
mandated the use of Dr. Posner’s system. The assessment found that the drug
doubled the risks of suicidal symptoms. In June, an F.D.A. advisory committee
voted unanimously that the agency reject rimonabant because of its psychiatric
effects, and Sanofi-Aventis withdrew the application although the drug is sold
in Europe.
Just this month, the results of a trial of Merck’s obesity drug, taranabant,
were published showing similar psychiatric problems. Meanwhile, fears have grown
that drugs used to treat epilepsy, seizures and mood disorders may have similar
effects. An extensive examination of these medicines by the drug agency should
be completed this year.
Suddenly, agency officials realized that multiple classes of medicines might
cause dangerous psychiatric problems.
“Clearly we were somewhat surprised when this signal emerged in the pediatric
antidepressant data,” said Dr. Thomas P. Laughren, director of the drug agency’s
division of psychiatry products. “So various groups within F.D.A. are now
looking at suicidality more broadly as a possible adverse event.”
The drug agency’s concerns are consistent with a growing body of research
confirming that behavior is heavily influenced not only by genes but also by
seemingly innocuous changes in body chemistry. Drugs not reaching the brain were
once thought to be largely free of mental effects.
“One lesson from pharmacology is that you can see effects on emotion and
cognition without the drug entering the brain if a drug leads to peripheral
changes in” other chemicals that enter the brain, said Dr. Thomas R. Insel,
director of the National Institute of Mental Health.
Some critics say that the agency’s new-found focus on psychiatric side effects
is long overdue.
“The list of drugs that causes psychiatric problems is a very long one,” said
Dr. Sidney M. Wolfe, director of Public Citizen’s health research group.
Medicines to treat acne, hypertension, high cholesterol, swelling, heartburn,
pain, bacterial infections and insomnia can all cause psychiatric problems,
effects that were discovered in most cases after the drugs were approved and
used in millions of patients.
Some drugs cause depression so often that doctors prescribe antidepressants
prophylactically with them.
Among medicines still for sale, the F.D.A. has determined that the drugs’
benefits outweigh their psychiatric risks. Still, the agency now wants to
uncover such problems more reliably and before approval.
There are two reasons that the F.D.A. for years was inattentive to the
psychiatric effects of new medicines. First, distinguishing between mental
problems that spring from a disease and those that result from its treatment is
often difficult. For antidepressants, many researchers suggested that suicidal
behaviors resulted because, as patients’ depression lifted, they suddenly had
the energy to carry out previous suicidal thoughts.
Second, drug side effects are often first identified in clinical trials when
multiple doctors treating hundreds of patients record similar problems in trial
notes. But terms to describe depression or suicidal thoughts can vary widely,
making them hard to discern.
“The whole spectrum of suicidal thoughts, ideation and attempts is much more
difficult to define and study than” other drug problems, said Dr. Eric Colman,
deputy director of the drug agency’s division of metabolic and endocrine
products.
Indeed, the agency’s initial review of the effects of antidepressants in
children was plagued by inconsistent and erroneous observations by investigators.
A 10-year-old boy who tried to hang himself was listed only as having a
“personality disorder,” an overdose of 11 tablets was called a “medication error”
and a girl who slapped herself in the face was labeled as having attempted
suicide.
Dr. Posner’s team spent months reclassifying these events as either a suicidal
symptom or not. The team created a detailed questionnaire called the Columbia
Suicide Severity Rating Scale, now adopted by the drug agency as an often
mandatory test to be used in clinical trials.
The last time one medicine’s side effect led the F.D.A. to broadly re-examine
its drug approval process was in 1992, when it discovered that Seldane, a
popular antihistamine, could cause dangerous heart arrhythmias. Tests revealed
other drugs that could affect heart rhythms, and the agency soon mandated that
nearly all experimental medicines be tested for heart rhythm effects.
Unlike the Seldane example, however, not every experimental drug program must
use the new suicidal symptoms scale. Drug officials said that they looked at a
drug’s molecular structure and its effects in animals before deciding whether to
insist on the new test.
“That’s where it gets tricky,” said Dr. Colman. “It’s difficult to say where you
draw the line.”
But Dr. Posner said in an interview that so many companies and academic research
programs were adopting the suicide questionnaire that she was having trouble
keeping up with the demand for its use. The questionnaire has been translated
into 80 languages, and Dr. Posner has trained scores of teams of investigators
from around the world on how to use it. On Jan. 4 she lectured a group of
investigators at Yale.
Benjamin A. Toll, an assistant professor in the university’s department of
psychiatry, was in the audience and said he planned to use the Columbia
questionnaire in a trial almost immediately.
“It’s much more detailed than what we were doing before,” Dr. Toll said. “We
used to ask, ‘Are you feeling down? Are you feeling sad?’ ”
Dr. Colman said that the new questionnaire, while important, would not end the
uncertainty around suicidal symptoms.
“If a drug makes people depressed but doesn’t make them suicidal, what do you
conclude?” he asked. “There will always be some degree of uncertainty.”
F.D.A. Requiring
Suicide Studies in Drug Trials, NYT, 24.1.2008,
http://www.nytimes.com/2008/01/24/washington/24fda.html?hp
Heart disease deaths plummet
ahead of 2010 goal
23 January 2008
USA Today
By Steve Sternberg
Heart disease deaths in the USA have fallen below the American Heart
Association's prevention goal for 2010, and deaths from strokes are nearing
their own record low, the AHA said Tuesday.
But epidemics of diabetes, obesity and inactivity, along with widespread
racial, economic and geographic differences in access to care, threaten those
gains, warns AHA president Daniel Jones.
"Unless we can find a new strategy to stem diabetes and obesity, we can
anticipate a new wave of cardiovascular disease deaths," Jones says. He noted
that heart disease is still the nation's leading killer, and stroke ranks third.
New government data show that heart disease death rates dropped 25.8% between
1999 and 2005, from 195 to 144 deaths for every 100,000 people, surpassing the
AHA's 25% target reduction. Stroke deaths dropped 24.4%, from 61 to 47 deaths
per 100,000.
That adds up to roughly 160,000 lives saved in 2005, Jones says. If the trend
holds, the AHA projects that as many as 240,000 lives may be saved this year.
The analysis of data released by the National Center for Health Statistics
doesn't explain why death rates continue to fall. Studies suggest people are
eating better, smoking less and getting better medical care than Americans of
previous generations, says Paul Ridker of Brigham and Women's Hospital in
Boston.
Ridker says improved methods of preventing and treating cardiovascular disease
have paid off. "Not only have they reduced the number of events, but when events
occur, we're more likely to survive them," he says.
These advances didn't benefit everyone, AHA notes. The death rate for blacks
dropped by 23.8%, compared with 25.6% for whites. "While overall statistics look
better for the U.S. as a whole," Ridker says, "a major portion of our population
is not benefiting from this shift."
Heart disease death rates fell among women by 26.9%, and stroke deaths among
women were down 23.7%.
Signs of trouble loom on the horizon, among them twin epidemics of diabetes and
obesity in young people, says Daniel Levy of the National Heart, Lung, and Blood
Institute's Framingham study, a 50-year-old examination of heart disease in a
Massachusetts community.
"We haven't yet paid the full price in heart disease and stroke deaths for the
obesity epidemic in our children that began 25 years ago," he says.
Heart disease deaths
plummet ahead of 2010 goal, UT, 22.1.2008,
http://www.usatoday.com/news/health/2008-01-22-heart-disease_N.htm
Letters
Fibromyalgia: The Pain Is Very
Real
January 17,
2008
The New York Times
To the
Editor:
“Drug Approved. Is Disease Real?” (front page, Jan. 14) does a disservice to
your readers, including the millions of patients afflicted by fibromyalgia, a
debilitating condition. The fact that Western medicine does not yet understand a
condition does not make it any less “real.”
Millions of people suffer from the physical pain and crippling fatigue
associated with fibromyalgia. We are not hypochondriacs, but sick people in
search of a cure, and of more compassionate medical care.
Would that it were true that fibromyalgia patients “obsess over aches that other
people simply tolerate”; in truth, they suffer from pain other people can
scarcely imagine. To imply, as the article does, that doctors who advocate on
behalf of these patients are somehow “in the pocket” of the pharmaceutical
industry is to betray a stunning degree of cynicism, and of callow disregard for
the real lives and deep suffering of millions of human beings.
Shai Held
New York, Jan. 14, 2008
•
To the Editor:
The pain of fibromyalgia is real, even if some doctors don’t think it is a
disease. Fibromyalgia and the related chronic fatigue are syndromes, not
discrete diseases. Because there is no single test to identify them does not
make them a fiction in the mind of the sufferer.
The pain and discomfort experienced are similar to what ordinary people feel
when they have the flu. These are autoimmune disorders, with the exact
triggering mechanisms still unknown. There is no cure. Only time and a lower
stress lifestyle help.
I am a retired farmer who developed chronic fatigue and fibromyalgia through
exposure to grain dust and mold spores. My pain level comes and goes based on my
stress level and exposure to airborne proteins and smoke. I have a high pain
tolerance, and I take no drugs. When the pain comes, I accept it, and when it
goes away, I’m relieved. But it is real.
Fred Schumacher
Mankato, Minn., Jan. 14, 2008
•
To the Editor:
Your article suggesting that fibromyalgia isn’t a disease translates a
significant health problem into a polemic. The problem derives from medical
materialism. By this I mean that doctors tell patients that nothing’s wrong, if
no abnormality can be found.
With this stance, patients fall between the cracks of classic medicine left on
their own or to the burgeoning alternative medicine industry.
When I took the Hippocratic oath, I didn’t pledge to care for only patients with
stroke or cancer but instead to do whatever possible to reduce suffering and
improve health. Your article will make doctors, relatives and friends of
millions with fibromyalgia conclude that their symptoms are just a “physical
response to stress, depression, and economic and social anxiety.”
This is an opinion ignoring published medical literature showing brain
abnormalities in fibromyalgia and drugs that clearly improve patient health.
What’s needed is less talk and more federally financed, peer-reviewed research.
Benjamin H. Natelson
Newark, Jan. 15, 2008
The writer, a physician, is a professor of neurosciences and director of the
Pain and Fatigue Study Center at U.M.D.N.J.-New Jersey Medical School.
•
To the Editor:
As a psychiatrist, I am painfully familiar with the rhetorical wars regarding
what does or does not count as “a disease.” Historically, the concept of disease
arose in order to explain prolonged suffering and incapacity in the absence of
an obvious external cause, such as a knife wound. The word itself originally
denoted a state of “dis-ease.”
A number of conditions in medicine, psychiatry and neurology (including many
types of headache) create considerable suffering and incapacity, even though “no
biological tests exist to diagnose” them, and even when “the condition cannot be
linked to any environmental or biological causes.”
Those who are afflicted with such conditions deserve whatever safe forms of
treatment are most helpful to them, including medication and psychosocial
support. For these individuals, their “dis-ease” is all too real.
Ronald Pies
Lexington, Mass., Jan. 14, 2008
•
To the Editor:
Your article is indeed a milestone for the fibromyalgia community and the
millions of Americans who suffer from this chronic pain disorder. We are glad
that The Times is shedding light on this medical condition on its front page.
But the article presents outdated opinions and doesn’t discuss the research
advances of the last decade by institutions like Johns Hopkins University, the
University of Michigan, the National Institutes of Health and the Food and Drug
Administration. Instead, you chose to focus on the opinions of a few medical
outsiders who still question the legitimacy of fibromyalgia.
We at the National Fibromyalgia Association felt hopeful that the misperceptions
and days of patient ridicule were behind us, but your article proves that we
still have a lot of work to do. Fortunately, we are more than up to the task.
Lynne Matallana
President and Founder, National Fibromyalgia Association
Anaheim, Calif., Jan. 14, 2008
•
To the Editor:
To continue attributing the painful symptoms of fibromyalgia to “stress,
depression, and economic and social anxiety” in an age that has abandoned
similar assumptions about ulcers and other ailments seems like anachronistic
scientific thought. This especially when a new pain treatment may hold promise.
But minimizing intractable pain, as do some doctors quoted in the article, by
chalking it up as an inability to adapt to the “vicissitudes” of life, surely
reveals less of the fibromyalgia patient’s temperament than his doctor’s.
Jane MacPherson
New York, Jan. 14, 2008
•
To the Editor:
Your article about the new fibromyalgia drug Lyrica may give hope to many women
suffering from this debilitating condition. Yet what we need to remember is that
medication is not the answer for everyone. I have suffered from fibromyalgia for
many years. After several different prescription painkillers, I decided to take
control of my situation.
I changed my eating habits, lost weight and took whole food supplements,
including fish oil. I have been symptom-free for several years, with occasional
brief relapses. Acupuncture has also been known to help.
The sad part is, most doctors will not advise women that there are other, safer
ways of handling fibromyalgia because it will be less money in their pockets.
Fibromyalgia is most definitely a real condition, but like many others we should
try a holistic approach before resorting to medication.
Marie Warmbrandt
Pembroke Pines, Fla., Jan. 16, 2008
Fibromyalgia: The Pain Is Very Real, NYT, 17.1.2008,
http://www.nytimes.com/2008/01/17/opinion/l17disease.html
Cholesterol as a Danger Has Skeptics
January 17,
2008
The New York Times
By ALEX BERENSON
For
decades, the theory that lowering cholesterol is always beneficial has been a
core principle of cardiology. It has been accepted by doctors and used by drug
makers to win quick approval for new medicines to reduce cholesterol.
But now some prominent cardiologists say the results of two recent clinical
trials have raised serious questions about that theory — and the value of two
widely used cholesterol-lowering medicines, Zetia and its sister drug, Vytorin.
Other new cholesterol-fighting drugs, including one that Merck hopes to begin
selling this year, may also require closer scrutiny, they say.
“The idea that you’re just going to lower LDL and people are going to get
better, that’s too simplistic, much too simplistic,” said Dr. Eric J. Topol, a
cardiologist and director of the Scripps Translational Science Institute in La
Jolla, Calif. LDL, or low-density lipoprotein, is the so-called bad cholesterol,
in contrast to high-density lipoprotein, or HDL.
For patients and drug companies, the stakes are enormous. Led by best sellers
like Lipitor from Pfizer, cholesterol-lowering medicines, taken by tens of
millions of patients daily, are the largest drug category worldwide, with annual
sales of $40 billion.
Despite widespread use of the drugs, though, heart disease remains the biggest
killer in the United States and other industrialized nations, and many people
still have cholesterol levels far higher than doctors recommend.
As a result, drug companies are investing billions of dollars in experimental
new cholesterol-lowering medicines that may eventually be used alongside the
existing drugs. If the new questions result in slower approvals, it would be yet
another handicap for the drug industry.
Because the link between excessive LDL cholesterol and cardiovascular disease
has been so widely accepted, the Food and Drug Administration generally has not
required drug companies to prove that cholesterol medicines actually reduce
heart attacks before approval.
They have not had to conduct so-called outcome or events trials beforehand,
which are expensive studies that involve thousands of patients and track whether
episodes like heart attacks are reduced.
So far, proof that a drug lowers LDL cholesterol has generally been enough to
lead to approval. Only then does the drug’s maker begin an events trial. And
until the results of that trial are available, a process that can take several
years, doctors and patients must accept the medicine’s benefits largely on
faith.
“You’ve got a huge chasm between F.D.A. licensure and a clinical events trial,”
said Dr. Allen J. Taylor, the chief of cardiology at Walter Reed Army Medical
Center.
Nonetheless, the multistep process has worked well for several cholesterol drugs
— including Lipitor and Zocor, which are in a class of drugs known as statins.
In those cases, the postapproval trials confirmed that the drugs reduce heart
attacks and strokes, adding to confidence about the link between cholesterol and
heart disease.
Doctors generally believe that the amount by which cholesterol is lowered, not
the method of lowering it, is what matters.
That continues to be the assumption of Dr. Scott M. Grundy, a professor of
medicine at the University of Texas Southwestern Medical Center who was the
chairman of a panel in 2001 that set national guidelines for cholesterol
treatment.
“LDL lowering, however it occurs, delays development of coronary atherosclerosis
and reduces risk for heart attack,” Dr. Grundy said this week. In
atherosclerosis, plaque builds up in the arteries, eventually leading to blood
clots and other problems that cause heart attacks and strokes.
In the last 13 months, however, the failures of two important clinical trials
have thrown that hypothesis into question.
First, Pfizer stopped development of its experimental cholesterol drug
torcetrapib in December 2006, when a trial involving 15,000 patients showed that
the medicine caused heart attacks and strokes. That trial — somewhat unusual in
that it was conducted before Pfizer sought F.D.A. approval — also showed that
torcetrapib lowered LDL cholesterol while raising HDL, or good cholesterol.
Torcetrapib’s failure, Dr. Taylor said, shows that lowering cholesterol alone
does not prove a drug will benefit patients.
Then, on Monday, Merck and Schering-Plough announced that Vytorin, which
combines Zetia with Zocor, had failed to reduce the growth of fatty arterial
plaque in a trial of 720 patients. In fact, patients taking Vytorin actually had
more plaque growth than those who took Zocor alone.
Despite those drawbacks, that trial, called Enhance, also showed that patients
on Vytorin had lower LDL levels than those on Zocor alone. For the second time
in just over a year, a clinical trial found that LDL reduction did not translate
into measurable medical benefits.
The Enhance trial was not an events trial and was not intended to study whether
Zetia or Vytorin were effective at reducing heart attacks. But the growth of
fatty plaque is closely correlated with heart attacks and strokes.
Without data from events trials for Zetia and Vytorin, no one can be certain if
the drugs help or hurt patients. But Merck and Schering did not begin an events
trial for the drugs until 2006, nearly four years after the F.D.A. approved
Zetia. That trial will not be completed until 2011.
Dr. Robert M. Califf, the vice chancellor for clinical research at Duke
University, and a co-lead investigator on the Zetia trial still under way, said
companies should have started the trials more quickly. “Outcome trials ought to
start when you know you’re going to get on the market,” he said.
On Tuesday, the American Heart Association called for the Zetia outcome trial to
be completed as quickly as possible.
Merck has asked the F.D.A. to approve its drug Cordaptive, which raises HDL
cholesterol and lowers LDL, without waiting for the results of an events trial.
Merck has begun an events trial for Cordaptive, but data will not be available
until 2013.
Merck has submitted the application for Cordaptive and has said it expects an
answer from the F.D.A. before July. Doctors, patients and the drug industry will
be waiting to see whether regulators are still willing to accept the theory that
lower cholesterol is always a good thing.
Cholesterol as a Danger Has Skeptics, NYT, 17.1.2008,
http://www.nytimes.com/2008/01/17/business/17drug.html
Antidepressant Studies Unpublished
January 17,
2008
The New York Times
By BENEDICT CAREY
The makers
of antidepressants like Prozac and Paxil never published the results of about a
third of the drug trials that they conducted to win government approval,
misleading doctors and consumers about the drugs’ true effectiveness, a new
analysis has found.
In published trials, about 60 percent of people taking the drugs report
significant relief from depression, compared with roughly 40 percent of those on
placebo pills. But when the less positive, unpublished trials are included, the
advantage shrinks: the drugs outperform placebos, but by a modest margin,
concludes the new report, which appears Thursday in The New England Journal of
Medicine.
Previous research had found a similar bias toward reporting positive results for
a variety of medications; and many researchers have questioned the reported
effectiveness of antidepressants. But the new analysis, reviewing data from 74
trials involving 12 drugs, is the most thorough to date. And it documents a
large difference: while 94 percent of the positive studies found their way into
print, just 14 percent of those with disappointing or uncertain results did.
The finding is likely to inflame a continuing debate about how drug trial data
is reported. In 2004, after revelations that negative findings from
antidepressant trials had not been published, a group of leading journals agreed
to stop publishing clinical trials that were not registered in a public
database. Trade groups representing the world’s largest drug makers announced
that members’ companies would begin to release more data from trials more
quickly, on their own database, clinicalstudyresults.org.
And last year, Congress passed legislation that expanded the type of trials and
the depth of information that must be submitted to clinicaltrials.gov, a public
database operated by the National Library of Medicine. The Food and Drug
Administration’s Web site provides limited access to recent reviews of drug
trials, but critics say it is very hard to navigate.
“This is a very important study for two reasons,” said Dr. Jeffrey M. Drazen,
editor in chief of The New England Journal. “One is that when you prescribe
drugs, you want to make sure you’re working with best data possible; you
wouldn’t buy a stock if you only knew a third of the truth about it.”
Second, Dr. Drazen continued, “we need to show respect for the people who enter
a trial.”
“They take some risk to be in the trial, and then the drug company hides the
data?” he asked. “That kind of thing gets us pretty passionate about this
issue.”
Alan Goldhammer, deputy vice president for regulatory affairs at the
Pharmaceutical Research and Manufacturers of America, said the new study
neglected to mention that industry and government had already taken steps to
make clinical trial information more transparent. “This is all based on data
from before 2004, and since then we’ve put to rest the myth that companies have
anything to hide,” he said.
In the study, a team of researchers identified all antidepressant trials
submitted to the Food and Drug Administration to win approval from 1987 to 2004.
The studies involved 12,564 adult patients testing drugs like Prozac from Eli
Lilly, Zoloft from Pfizer and Effexor from Wyeth.
The researchers obtained unpublished data on the more recently approved drugs
from the F.D.A.’s Web site. For older drugs, they tracked down hard copies of
unpublished studies through colleagues, or using the Freedom of Information Act.
They checked all of these studies against databases of published research, and
also wrote to the companies that conducted the studies to ask if specific trials
had been published.
They found that 37 of 38 trials that the F.D.A. viewed as having positive
results were published in journals. The agency viewed as failed or unconvincing
36 other trials, of which 14 made it into journals.
But 11 of those 14 journal articles “conveyed a positive outcome” that was not
justified by the underlying F.D.A. review, said the new study’s lead author, Dr.
Erick H. Turner, a psychiatrist and former F.D.A. reviewer who now works at
Oregon Health and Sciences University and the Portland Veterans Affairs Medical
Center. His co-authors included researchers at Kent State University and the
University of California, Riverside.
Dr. Turner said the selective reporting of favorable studies sets up patients
for disappointment. “The bottom line for people considering an antidepressant, I
think, is that they should be more circumspect about taking it,” he said, “and
not be so shocked if it doesn’t work the first time and think something’s wrong
with them.”
For doctors, he said, “They end up asking, ‘How come these drugs seem to work so
well in all these studies, and I’m not getting that response?’ ”
Dr. Thomas P. Laughren, director of the division of psychiatry products at the
F.D.A., said the agency had long been aware that favorable studies of drugs were
more likely to be published.
“It’s a problem we’ve been struggling with for years,” he said in an interview.
“I have no problem with full access to all trial data; the question for us is
how do you fit it all on a package insert,” the information that accompanies
many drugs.
Dr. Donald F. Klein, an emeritus professor of psychiatry at Columbia, said drug
makers were not the only ones who can be reluctant to publish unconvincing
results. Journals, and study authors, too, may drop studies that are
underwhelming.
“If it’s your private data, and you don’t like how it came out, well, we
shouldn’t be surprised that some doctors don’t submit those studies,” he said.
Antidepressant Studies Unpublished, NYT, 17.1.2008,
http://www.nytimes.com/2008/01/17/health/17depress.html
Drug
Approved. Is Disease Real?
January 14,
2008
The New York Times
By ALEX BERENSON
Fibromyalgia is a real disease. Or so says Pfizer in a new television
advertising campaign for Lyrica, the first medicine approved to treat the pain
condition, whose very existence is questioned by some doctors.
For patient advocacy groups and doctors who specialize in fibromyalgia, the
Lyrica approval is a milestone. They say they hope Lyrica and two other drugs
that may be approved this year will legitimize fibromyalgia, just as Prozac
brought depression into the mainstream.
But other doctors — including the one who wrote the 1990 paper that defined
fibromyalgia but who has since changed his mind — say that the disease does not
exist and that Lyrica and the other drugs will be taken by millions of people
who do not need them.
As diagnosed, fibromyalgia primarily affects middle-aged women and is
characterized by chronic, widespread pain of unknown origin. Many of its
sufferers are afflicted by other similarly nebulous conditions, like irritable
bowel syndrome.
Because fibromyalgia patients typically do not respond to conventional
painkillers like aspirin, drug makers are focusing on medicines like Lyrica that
affect the brain and the perception of pain.
Advocacy groups and doctors who treat fibromyalgia estimate that 2 to 4 percent
of adult Americans, as many as 10 million people, suffer from the disorder.
Those figures are sharply disputed by those doctors who do not consider
fibromyalgia a medically recognizable illness and who say that diagnosing the
condition actually worsens suffering by causing patients to obsess over aches
that other people simply tolerate. Further, they warn that Lyrica’s side
effects, which include severe weight gain, dizziness and edema, are very real,
even if fibromyalgia is not.
Despite the controversy, the American College of Rheumatology, the Food and Drug
Administration and insurers recognize fibromyalgia as a diagnosable disease. And
drug companies are aggressively pursuing fibromyalgia treatments, seeing the
potential for a major new market.
Hoping to follow Pfizer’s lead, two other big drug companies, Eli Lilly and
Forest Laboratories, have asked the F.D.A. to let them market drugs for
fibromyalgia. Approval for both is likely later this year, analysts say.
Worldwide sales of Lyrica, which is also used to treat diabetic nerve pain and
seizures and which received F.D.A. approval in June for fibromyalgia, reached
$1.8 billion in 2007, up 50 percent from 2006. Analysts predict sales will rise
an additional 30 percent this year, helped by consumer advertising.
In November, Pfizer began a television ad campaign for Lyrica that features a
middle-aged woman who appears to be reading from her diary. “Today I struggled
with my fibromyalgia; I had pain all over,” she says, before turning to the
camera and adding, “Fibromyalgia is a real, widespread pain condition.”
Doctors who specialize in treating fibromyalgia say that the disorder is
undertreated and that its sufferers have been stigmatized as chronic
complainers. The new drugs will encourage doctors to treat fibromyalgia
patients, said Dr. Dan Clauw, a professor of medicine at the University of
Michigan who has consulted with Pfizer, Lilly and Forest.
“What’s going to happen with fibromyalgia is going to be the exact thing that
happened to depression with Prozac,” Dr. Clauw said. “These are legitimate
problems that need treatments.”
Dr. Clauw said that brain scans of people who have fibromyalgia reveal
differences in the way they process pain, although the doctors acknowledge that
they cannot determine who will report having fibromyalgia by looking at a scan.
Lynne Matallana, president of the National Fibromyalgia Association, a patients’
advocacy group that receives some of its financing from drug companies, said the
new drugs would help people accept the existence of fibromyalgia. “The day that
the F.D.A. approved a drug and we had a public service announcement, my pain
became real to people,” Ms. Matallana said.
Ms. Matallana said she had suffered from fibromyalgia since 1993. At one point,
the pain kept her bedridden for two years, she said. Today she still has pain,
but a mix of drug and nondrug treatments — as well as support from her family
and her desire to run the National Fibromyalgia Association — has enabled her to
improve her health, she said. She declined to say whether she takes Lyrica.
“I just got to a point where I felt, I have pain but I’m going to have to figure
out how to live with it,” she said. “I absolutely still have fibromyalgia.”
But doctors who are skeptical of fibromyalgia say vague complaints of chronic
pain do not add up to a disease. No biological tests exist to diagnose
fibromyalgia, and the condition cannot be linked to any environmental or
biological causes.
The diagnosis of fibromyalgia itself worsens the condition by encouraging people
to think of themselves as sick and catalog their pain, said Dr. Nortin Hadler, a
rheumatologist and professor of medicine at the University of North Carolina who
has written extensively about fibromyalgia.
“These people live under a cloud,” he said. “And the more they seem to be around
the medical establishment, the sicker they get.”
Dr. Frederick Wolfe, the director of the National Databank for Rheumatic
Diseases and the lead author of the 1990 paper that first defined the diagnostic
guidelines for fibromyalgia, says he has become cynical and discouraged about
the diagnosis. He now considers the condition a physical response to stress,
depression, and economic and social anxiety.
“Some of us in those days thought that we had actually identified a disease,
which this clearly is not,” Dr. Wolfe said. “To make people ill, to give them an
illness, was the wrong thing.”
In general, fibromyalgia patients complain not just of chronic pain but of many
other symptoms, Dr. Wolfe said. A survey of 2,500 fibromyalgia patients
published in 2007 by the National Fibromyalgia Association indicated that 63
percent reported suffering from back pain, 40 percent from chronic fatigue
syndrome, and 30 percent from ringing in the ears, among other conditions. Many
also reported that fibromyalgia interfered with their daily lives, with
activities like walking or climbing stairs.
Most people “manage to get through life with some vicissitudes, but we adapt,”
said Dr. George Ehrlich, a rheumatologist and an adjunct professor at the
University of Pennsylvania. “People with fibromyalgia do not adapt.”
Both sides agree that people who are identified as having fibromyalgia do not
get much relief from traditional pain medicines, whether anti-inflammatory drugs
like ibuprofen — sold as Advil, among other brands — or prescription opiates
like Vicodin. So drug companies have sought other ways to reduce pain.
Pfizer’s Lyrica, known generically as pregabalin, binds to receptors in the
brain and spinal cord and seems to reduce activity in the central nervous
system.
Exactly why and how Lyrica reduces pain is unclear. In clinical trials, patients
taking the drug reported that their pain — whether from fibromyalgia, shingles
or diabetic nerve damage — fell on average about 2 points on a 10-point scale,
compared with 1 point for patients taking a placebo. About 30 percent of
patients said their pain fell by at least half, compared with 15 percent taking
placebos.
The F.D.A. reviewers who initially examined Pfizer’s application for Lyrica in
2004 for diabetic nerve pain found those results unimpressive, especially in
comparison to Lyrica’s side effects. The reviewers recommended against approving
the drug, citing its side effects.
In many patients, Lyrica causes weight gain and edema, or swelling, as well as
dizziness and sleepiness. In 12-week trials, 9 percent of patients saw their
weight rise more than 7 percent, and the weight gain appeared to continue over
time. The potential for weight gain is a special concern because many
fibromyalgia patients are already overweight: the average fibromyalgia patient
in the 2007 survey reported weighing 180 pounds and standing 5 feet 4 inches.
But senior F.D.A. officials overruled the initial reviewers, noting that severe
pain can be incapacitating. “While pregabalin does present a number of concerns
related to its potential for toxicity, the overall risk-to-benefit ratio
supports the approval of this product,” Dr. Bob Rappaport, the director of the
F.D.A. division reviewing the drug, wrote in June 2004.
Pfizer began selling Lyrica in the United States in 2005. The next year the
company asked for F.D.A. approval to market the drug as a fibromyalgia
treatment. The F.D.A. granted that request in June 2007.
Pfizer has steadily ramped up consumer advertising of Lyrica. During the first
nine months of 2007, it spent $46 million on ads, compared with $33 million in
2006, according to TNS Media Intelligence.
Dr. Steve Romano, a psychiatrist and a Pfizer vice president who oversees
Lyrica, says the company expects that Lyrica will be prescribed for fibromyalgia
both by specialists like neurologists and by primary care doctors. As doctors
see that the drug helps control pain, they will be more willing to use it, he
said.
“When you help physicians to recognize the condition and you give them
treatments that are well tolerated, you overcome their reluctance,” he said.
Both the Lilly and Forest drugs being proposed for fibromyalgia were originally
developed as antidepressants, and both work by increasing levels of serotonin
and norepinephrine, brain transmitters that affect mood. The Lilly drug,
Cymbalta, is already available in the United States, while the Forest drug,
milnacipran, is sold in many countries, though not the United States.
Dr. Amy Chappell, a medical fellow at Lilly, said that even though Cymbalta is
an antidepressant, its effects on fibromyalgia pain are independent of its
antidepressant effects. In clinical trials, she said, even fibromyalgia patients
who are not depressed report relief from their pain on Cymbalta.
The overall efficacy of Cymbalta and milnacipran is similar to that of Lyrica.
Analysts and the companies expect that the drugs will probably be used together.
“There’s definitely room for several drugs,” Dr. Chappell said.
But physicians who are opposed to the fibromyalgia diagnosis say the new drugs
will probably do little for patients. Over time, fibromyalgia patients tend to
cycle among many different painkillers, sleep medicines and antidepressants,
using each for a while until its benefit fades, Dr. Wolfe said.
“The fundamental problem is that the improvement that you see, which is not
really great in clinical trials, is not maintained,” Dr. Wolfe said.
Still, Dr. Wolfe expects the drugs will be widely used. The companies, he said,
are “going to make a fortune.”
Drug Approved. Is Disease Real?, NYT, 14.1.2008,
http://www.nytimes.com/2008/01/14/health/14pain.html?ref=opinion
Editorial
H.I.V. Rises Among Young Gay Men
January 14, 2008
The New York Times
AIDS appears to be making an alarming comeback. The Journal of the American
Medical Association reports that the incidence of H.I.V. infection among gay men
is shooting up, following an encouraging period of decline. The rise of
infections among younger gay men, especially black and Hispanic men, is
troubling, and the study carries the clear implication that people at high risk
of contracting the disease are becoming less cautious.
Statistics gathered by New York City health officials show that new diagnoses of
H.I.V. infection — the virus that causes AIDS — in gay men under age 30 rose 32
percent between 2001 and 2006. Among black and Hispanic men, the figure was 34
percent. Most troubling, the number of new diagnoses among the youngest men in
the study, those between ages 13 and 19, doubled.
New York officials say increased alcohol and drug use may be partly responsible
since they make unprotected sex more likely. Other basic precautions, including
finding out whether a potential partner is infected, are also apparently being
ignored.
The one bright spot in this bleak picture was the 22 percent decline in
infections among men over 30 in the New York study. Awareness of the disease’s
devastating effects, as much as maturity, may explain the difference. A large
number of these older men came of age when AIDS was all but untreatable. They
may have buried friends who died after being horribly ill.
When the disease was new and terrifying, the gay community helped change
behavior by preaching loudly against taking sexual risks. From San Francisco to
New York, bathhouses notorious for promoting casual sex changed the way they did
business or closed down. Condoms were encouraged, and so was H.I.V. testing.
“Silence equals death” was the motto of the day.
Silence now seems to be winning the day. Nearly 6,000 gay men died of AIDS in
the United States in 2005; still, many young men appear to have persuaded
themselves that the infection is no longer such a big deal. It is true that
antiretroviral therapy has improved the outlook for anyone who becomes infected.
But the treatments are still too new to know whether they can work much beyond a
decade. Public health officials need to continue to distribute condoms,
encourage testing and treat those who are ill. Leaders in the hardest-hit
communities need to start speaking out again. The fight against AIDS is far from
over.
H.I.V. Rises Among Young
Gay Men, NYT, 14.1.2008,
http://www.nytimes.com/2008/01/14/opinion/14mon2.html?ref=opinion
Team
Creates Rat Heart Using Cells of Baby Rats
January 14,
2008
The New York Times
By LAWRENCE K. ALTMAN
Medicine’s
dream of growing new human hearts and other organs to repair or replace damaged
ones received a significant boost Sunday when University of Minnesota
researchers reported success in creating a beating rat heart in a laboratory.
Experts not involved in the Minnesota work called it “a landmark achievement”
and “a stunning” advance. But they and the Minnesota researchers cautioned that
the dream, if it is ever realized, was still at least 10 years away.
Dr. Doris A. Taylor, the head of the team that created the rat heart, said she
followed a guiding principle of her laboratory: “give nature the tools, and get
out of the way.”
“We just took nature’s own building blocks to build a new organ,” Dr. Taylor
said of her team’s report in the journal Nature Medicine.
The researchers removed all the cells from a dead rat heart, leaving the valves
and outer structure as scaffolding for new heart cells injected from newborn
rats. Within two weeks, the cells formed a new beating heart that conducted
electrical impulses and pumped a small amount of blood.
With modifications, scientists should be able to grow a human heart by taking
stem cells from a patient’s bone marrow and placing them in a cadaver heart that
has been prepared as a scaffold, Dr. Taylor said in a telephone interview from
her laboratory in Minneapolis. The early success “opens the door to this notion
that you can make any organ: kidney, liver, lung, pancreas — you name it and we
hope we can make it,” she said.
Todd N. McAllister of Cytograft Tissue Engineering in Novato, Calif., said,
“Doris Taylor’s work is one of those maddeningly simple ideas that you knock
yourself on the head, saying, ‘Why didn’t I think of that?’ ” Dr. McAllister’s
team has used a snippet of a patient’s skin to grow blood vessels in a
laboratory, and then implanted them to restore blood flow around a patient’s
damaged arteries and veins.
The field of tissue engineering has been growing rapidly. For many years,
doctors have used engineered skin for burn patients. Engineered cartilage is
used for joint repairs. Researchers are investigating the use of stem cells to
repair cardiac muscle damaged by heart attacks. Also, new bladders grown from a
patient’s own cells are being tested in the same patients.
Dr. Taylor is a newcomer to tissue regeneration. She began her professional
career at the Albert Einstein College of Medicine in the Bronx investigating
gene therapy and then cell therapy. She said she switched to tissue regeneration
when she realized the limiting step in trying to generate an organ was not the
number of cells needed, but the complexity of creating a three-dimensional
structure.
“The heart is a beautiful organ,” Dr. Taylor said, “and it’s not one that I
thought I’d ever be able to build in a dish.”
Her view changed about three years ago when she recalled that cells were removed
from human and pig heart valves before they were used to replace damaged human
ones. As she contemplated replacing the old rat cells with new ones, Dr. Taylor
followed another of her mantras: “Trust your crazy ideas.”
Progress came in fits and starts. “We made every mistake known, did every
experiment wrong and had to go back and do them right,” Dr. Taylor said.
She poured detergents like those in shampoos in the rat’s arteries to wash out
the heart cells and then injected neonatal cardiac cells. The first two
detergents she tested failed. But a third concoction led to a clear, translucent
scaffold that retained the heart’s architecture.
After injecting the young rat heart cells into a scaffold, she stimulated them
electrically and created an artificial circulation as the equivalent of blood
pressure to make the heart pump and produce a pulse. The steps also helped the
cells mature. Tests like examining slices of the heart under a microscope showed
they were living cells.
To test the biological compatibility of the new hearts, the team transplanted
them into the abdomen of unrelated live rats. The hearts were not immediately
rejected. A blood supply developed. The hearts beat regularly. And cells from
the host rats moved in and began to reline the blood vessels, even growing in
the wall of the hearts.
Dr. Taylor is now conducting similar experiments on pigs as a step toward human
work. “Working out the details in a pig heart made a lot more sense” because the
anatomy of the porcine heart is the closest to humans and pigs are plentiful,
she said.
“The next goal will be to see if we can get the heart to pump strongly enough
and become mature enough that we can use it to keep an animal alive” in a
replacement transplant, Dr. Taylor said.
As for human hearts, the best-case situation would be to obtain them from
cadavers, remove their cells to make a scaffold and then inject bone marrow,
muscle or young cardiac cells from a patient. The process of repopulating the
scaffold with new cells would take a few months, she said.
The body replaces its proteins every few months, so the hope is that the body
will create a matrix that it recognizes as its own.
One potential problem is that antirejection drugs might be required to prevent
adverse immune reactions from the scaffold. In that case, Dr. Taylor hopes such
therapy would be needed only temporarily.
Many things that work in experiments on animals fail in humans because of the
species barrier. Dr. McAllister said that in Dr. Taylor’s case “the principal
problem in escalating it to humans is one of scale, not of cell biology, and
that is an easier problem to solve potentially.”
Dr. Taylor said, “If it works, it means that there will be many more organs
available for transplants.”
Because the components of the biologic matrix differ for every organ, Dr. Taylor
expects that scientists will be able to do tests to answer two fundamental
questions: Can a stem cell be placed anywhere in the body and still produce a
heart, kidney or other organ? Or must a stem cell be placed in its anatomic
position to do so?
Such tests might include taking stem cells from one organ, for example a kidney,
and putting them in a kidney, liver or heart to begin to understand if the stem
cells are innately committed to produce kidneys or whether they will convert to
produce livers or hearts.
Beginning Jan. 15, Adam Liptak’s column, “Sidebar,” will appear on Tuesdays. Dan
Barry’s column, “This Land,” will return on Monday, Jan. 21.
Team Creates Rat Heart Using Cells of Baby Rats, NYT,
14.1.2008,
http://www.nytimes.com/2008/01/14/health/14heart.html
NYC
Death Rate Hit All - Time Low in '06
January 8,
2008
Filed at 7:39 p.m. ET
By THE ASSOCIATED PRESS
The New York Times
NEW YORK
(AP) -- The city's overall death rate dropped to an all-time low in 2006 due in
part to declines in mortality from HIV and smoking-related illness, the health
commissioner said Tuesday.
The number of deaths fell to 55,391 in 2006 from 57,068 a year earlier,
according to the city's Health Department of Health and Mental Hygiene. The only
leading killer that increased significantly was substance use, up 8 percent.
Heart disease and cancer remained the most deadly, claiming 21,844 and 13,116
lives, respectively.
Between 2005 and 2006, death from HIV fell almost 15 percent, from 1,419 to
1,209, reflecting the lowest numbers since 1984 when 952 deaths from AIDS were
recorded citywide.
Researchers attributed the decline to lower infection rates because of syringe
exchange programs, expanded HIV testing, and slower disease progression.
HIV mortality remains concentrated among the city's minority populations, with
roughly 34 percent of deaths among black men; 21 percent among black women; 11
percent among white men; and 3 percent among white women.
New HIV diagnoses have recently increased among young men who have sex with men,
but the trend has yet to affect mortality rates.
All smoking-related deaths dropped 11.2 percent between 2002 and 2006, from
8,722 to 7,744. The figures do not include deaths from exposure to second-hand
smoke.
The report also showed that life expectancy for women between 2004 and 2005 rose
by 2.5 months to 81.3 years, while male life expectancy remained unchanged at
75.7 years. Overall life expectancy rose to 78.7 years from 78.6 years.
------
On the Net:
Vital Statistics Annual Summaries:
http://www.nyc.gov/html/doh/html/vs/vs.shtml
NYC Death Rate Hit All - Time Low in '06, NYT, 8.1.2008,
http://www.nytimes.com/aponline/world/AP-NYC-Death-Rate.html
To
Gephyrophobiacs, Bridges Are a Terror
January 8,
2008
The New York Times
By LISA W. FODERARO
The
Verrazano-Narrows bridge has been called a study in grace.
For Jan Steers, it was a study in terror.
Even thinking about driving across the 4,260-foot suspension span made her start
to feel dizzy, made her heart race, her breath tightening into short rapid
gasps.
Mrs. Steers, 47, suffered from a little-known disorder called gephyrophobia, a
fear of bridges. And she had the misfortune of living in a region with 26 major
bridges, whose heights and spans could turn an afternoon car ride into a rolling
trip through a haunted house.
Some people go miles out of their way to avoid crossing the George Washington
Bridge — for example, driving to Upper Manhattan from Teaneck, N.J., by way of
the Lincoln Tunnel, a detour that can stretch a 19-minute jog into a
three-quarter-hour ordeal. Other bridge phobics recite baby names or play the
radio loudly as they ease onto a nerve-jangling span — anything to focus the
mind. Still others take a mild tranquilizer an hour before buckling up to cross
a bridge.
The Tappan Zee Bridge, rising more than 150 feet over the Hudson River, appears
to inspire particular panic — so much so that New York State offers the skittish
a chauffeur who will transport them across the span.
Similar rescue measures are provided in other places around the country with
especially fearsome bridges. Authorities at the San Francisco-Oakland Bay
Bridge, for example, will dispatch a tow truck to pull panic-stricken drivers to
the other side. The Mackinac Bridge, connecting Michigan’s Lower and Upper
Peninsulas, provides a transport service like the Tappan Zee’s. Mrs. Steers’s
phobia was so severe that she was virtually trapped on Staten Island for 13
years. She missed her brother’s wedding in Brooklyn. She sent her husband and
two children off on family vacations without her. She had never seen her
sister’s house at the Jersey Shore.
“Every time I thought about going over a bridge I would get terrible, terrible
anxiety,” said Mrs. Steers, 47, a former nursing home housekeeper. “That’s when
my world started getting smaller and smaller.”
Dr. Michael R. Liebowitz, a professor of clinical psychiatry at Columbia
University, said that while fear of flying is widely accepted, especially in the
wake of Sept. 11, the fear of crossing bridges is less well known and still
“carries a stigma.”
There are no exact numbers of how many people suffer from the disorder, he said,
adding that it is not only common but treatable.
“It’s not an isolated phobia, but usually part of a larger constellation,” said
Dr. Liebowitz, founder of the Anxiety Disorders Clinic at the New York State
Psychiatric Institute. “It’s people who get panic attacks. You get light-headed,
dizzy; your heart races. You become afraid that you’ll feel trapped.”
The flip side of bridge phobia, which experts say is often related to a fear of
heights or open spaces, is a dread of driving through tunnels, more often linked
to claustrophobia, experts say. Some people suffer from one fear or the other;
some struggle with both. Whatever the cause, such phobias lead to panicky
feelings that sufferers go to great lengths to avoid, grinding normal routines
to a halt.
In the case of Mrs. Steers, who in the last three months has finally ventured
off Staten Island (with the help of behavioral therapy and medication), her
bridge-and-tunnel phobia was paralyzing. For others, the fear of bridges becomes
simply a somewhat embarrassing, highly uncomfortable backdrop to their lives.
Jane Cameron, a 60-year-old bereavement counselor and artist in
Hastings-on-Hudson, N.Y., loathes driving over bridges, but she has not let it
stop her. Nor has she sought help. For a time, she even had to drive across the
Tappan Zee every weekend en route to a country house she and her husband, Jamie,
owned in Sullivan County. “I would just grin and bear it,” she said.
She traces her lifelong fear to an early childhood experience. “One of my first
memories was going over the Brooklyn Bridge with my parents and looking out the
window and thinking, ‘Holy cow. It’s just me and the water and not enough in
between,’” she said. “I do have a feeling that I was pushed off a high bridge in
a past life.”
Her fear of bridges was put to the ultimate test in March when the couple
traveled to New Zealand, going on a trek through the mountains. She was forced
to walk across a dozen pedestrian bridges that wobbled high above the ground as
a storm raged.
“It was straight out of my worst nightmare,” she said. “I was practically sick
to my stomach. It was howling wind and rain, and there were swinging wooden
bridges with slats that were really, really high up. Nobody else seemed to be as
scared as I was.”
In hindsight, Ms. Cameron said, imagining the worst was therapeutic. “I felt
really good about it,” she said.
Then there are those who seem to have the most difficulty with bridges while on
foot, whether a simple downtown overpass or an interior walkway. Vicki
Shipkowitz, who works for a software company in San Francisco, attributes her
bridge jitters to a fear of heights. The more vivid the view from the bridge,
the greater her discomfort.
One place she hates to tread is a metal walkway leading to an exhibition space
on the sixth floor of the San Francisco Museum of Modern Art. Ms. Shipkowitz is
a member of the board of directors of ArtSpan, a nonprofit arts organization,
and she finds herself at the museum at least once a month.
“It’s got metal slats and you look all the way down to the ground floor,” she
said of the walkway. “I literally close my eyes and have someone lead me across.
If I go on my own, I don’t go across the bridge.”
In the New York region, the New York Thruway Authority will lead bridge phobics
over the Tappan Zee, the longest span in the state. A reluctant driver can call
the authority in advance and arrange to be driven across the bridge in his or
her own car by a patrol operator. The authority receives a half dozen such
requests a year, officials there say.
Ramesh Mehta, a division director for the authority, said the service helped
prevent situations in which a phobic driver might get stuck mid-span. “It is
very dangerous to stop the car right there on the bridge, because the traffic is
so great and somebody can get rear-ended,” he said.
Steve Coleman, a spokesman for the Port Authority of New York and New Jersey,
said that the agency did not have a policy in place to escort drivers through
the Holland and Lincoln Tunnels or across its four bridges, including the George
Washington.
For those determined to conquer — or at least tame — their fears, however, there
is ample help available: phobia workshops, exposure therapy, mental tricks,
medication, self-help books.
“Once you finally decide to fight it, you have to make sure you have the proper
tools in your bag,” said a 35-year-old financial services executive in Fairfield
County in Connecticut, who spoke on the condition of anonymity so as not to
jeopardize her work. For years, she avoided planes, trains, tunnels and traffic
jams. Sept. 11 intensified her fears. “It’s the whole trapped feeling you get,”
she said. “That’s the consistent vibe.”
In the last year, she began treatment at the Anxiety and Phobia Treatment Center
at White Plains Hospital Center, starting first with trains and recently moving
on to tunnels. In the last few months, she successfully traversed the Holland
and Lincoln Tunnels, with her counselor at her side.
Among her “tools” were such distractions as reciting baby names, reading license
plates backward and listening for words on the radio starting with the letter A.
“You want to engage your brain in another activity,” she said.
After many false starts, Mrs. Steers of Staten Island realized that she needed
more than distractions to help her overcome her bridge phobia. For several
years, in addition to receiving therapy through Freedom From Fear, a nonprofit
mental health organization based on Staten Island, she had taken an
antidepressant to relieve her anxiety. Still, she could not approach a bridge.
“Just the thought of going over a bridge would give me a panic attack,” she
said. “My husband and kids came to accept it, but it wasn’t easy. Two years ago,
I said I’ve had enough. I can’t keep doing this.”
Mary Guardino, founder and executive director of Freedom From Fear, knew about
Mrs. Steers’s struggles. Mrs. Guardino herself had suffered from panic attacks
for years, once abandoning her car on the Brooklyn Bridge and fleeing. “I said,
‘Take the tranquilizer, come to my office and I’ll take you over the Bayonne
Bridge,’” she said, recalling a conversation with Mrs. Steers.
On Sept. 20, Mrs. Steers took a small dose of Ativan, a tranquilizer, and got in
the car with Mrs. Guardino, who was the driver, and a nurse. She was armed with
a video recorder to tape her ride. “I went off Staten Island for the first time
in 13 years, and I did O.K.,” she said.
She has since crossed several bridges with her husband, driving the car herself
three times. She has gone shopping in Brooklyn and finally visited the house in
Red Bank, N.J., where her sister has lived for nine years, surprising her one
day on the doorstep. Still on the horizon are her brother’s house in Tappan,
N.Y., and the Brooklyn-Battery Tunnel.
“Oh, God,” she said. “Tunnels are even worse. I haven’t been to Manhattan yet.
That’s another thing on the list. But my ultimate goal is going on vacation with
my husband.”
To Gephyrophobiacs, Bridges Are a Terror, NYT, 8.1.2008,
http://www.nytimes.com/2008/01/08/nyregion/08bridge.html
Healthy
Habits Can Mean 14 Extra Years
January 8,
2008
Filed at 12:31 p.m. ET
By THE ASSOCIATED PRESS
The New York Times
LONDON (AP)
-- To get an extra 14 years of life, don't smoke, eat lots of fruits and
vegetables, exercise regularly and drink alcohol in moderation.
That is according to a study published Monday in the Public Library of Science
Medicine journal.
After tracking more than 20,000 people aged 45 to 79 years in the United Kingdom
from about 1993 to 2006, Kay-Tee Khaw of the University of Cambridge and
colleagues found that people who adopted these four healthy habits lived an
average of 14 years longer than those who didn't.
''We've known for a long time that these behaviors are good things to do, but
we've never seen these additive benefits before,'' said Susan Jebb, head of
Nutrition and Health at Britain's Medical Research Council. Jebb was not
involved in the study.
''Just doing one of these behaviors helps, but every step you make to improve
your health seems to have an added benefit,'' she said. The benefits were also
seen regardless of whether or not people were fat and what social class they
came from.
Study participants scored a point each for not smoking, regular physical
activity, eating five servings of fruits and vegetables a day and moderate
alcohol intake. People who scored four were four times less likely to die than
those who scored zero. Researchers tracked deaths from all causes, including
cardiovascular disease, cancer and respiratory diseases.
Participants filled in a health questionnaire and nurses conducted a medical
exam at a clinic. The study was largely paid for by the Medical Research Council
and Cancer Research United Kingdom.
Khaw said that the study should convince people that improving their health does
not always require extreme changes to their lifestyles. ''We didn't ask these
people to do anything exceptional,'' Khaw said. We measured normal behaviors
that were entirely feasible within people's normal, everyday lives.''
Public health experts said they hoped the study would inspire governments to
introduce policies helping people to adopt these changes.
''This research is an important piece of work which emphasizes how modifying
just a few risk factors can add years to your life,'' said Dr. Tim Armstrong, a
physical activity expert at the World Health Organization.
But because the study only observed people rather than testing specific changes,
experts said that it would be impossible to conclude that people who suddenly
adopted these healthy behaviors would automatically gain 14 years.
''We can't say that any one person could gain 14 years by doing these things,''
said Dr. Tim Armstrong, a physical activity expert at the World Health
Organization. ''The 14 years is an average across the population of what's
theoretically possible.''
Experts are also unsure if these new findings will actually improve the public's
health.
''What stops people from changing their behavior is not a lack of knowledge,''
Jebb said.
''Most people know that things like a good diet matter and that smoking is not
good for you,'' she said. ''We need to work on providing people with much more
practical support to help them change.''
Healthy Habits Can Mean 14 Extra Years, NYT, 8.1.2008,
http://www.nytimes.com/aponline/world/AP-Britain-Live-Longer.html
Racial
disparities persist in U.S. cancer treatment
Mon Jan 7,
2008
1:51am EST
Reuters
By Will Dunham
WASHINGTON
(Reuters) - U.S. blacks continue to get inferior cancer treatment compared to
whites, researchers said on Monday in a study showing that disparities first
documented in the early 1990s persist despite efforts to erase them.
The researchers assessed the type of treatment given to more than 143,000
Americans over age 65 for lung, breast, colon, rectal and prostate cancer from
1992 to 2002 under the Medicare government health insurance program.
Black patients were consistently less likely than whites to receive the
recommended types of treatment, the study found, and the problem was just as bad
in 2002 as in 1992.
The findings were published in the journal Cancer, published by the American
Cancer Society.
"What we found was that the racial disparities did not change during that
10-year time interval," Dr. Cary Gross of the Yale University School of Medicine
in New Haven, Connecticut, who led the study, said in a telephone interview.
Despite the publication of studies in the early 1990s documenting the
disparities and despite steps taken by some doctors and hospitals to understand
and address the problem, the study found little in the way of progress.
The reasons for racial disparities in cancer care and many other areas of health
care in the United States remain a contentious issue that touches on the
question of whether outright racism exists in the U.S. medical system.
"This sort of thing has been a problem in the United States for a long, long
time," Dr. Otis Brawley, chief medical officer of the American Cancer Society,
said in a telephone interview.
"I think individual racism likely accounts for a small amount of it, but not a
large amount. What I would refer to as institutional or societal racism accounts
for a much larger component of it," Brawley added, referring to enduring
educational and socioeconomic inequities faced by U.S. blacks.
SOCIETAL
INEQUITIES
The disparities were widest in lung, colon and rectal cancer in the study period
of 1992 to 2002.
Among patients with early-stage lung cancer, blacks were 19 percent less likely
than whites to get surgical removal of the tumor. Blacks with rectal cancer were
27 percent less likely to get additional chemotherapy to get rid of any
remaining cancer cells after surgical removal of a tumor. And blacks with colon
cancer were 24 percent less likely to get such chemotherapy.
Among breast cancer patients who had a lumpectomy, black women were 7 percent
less likely than whites to get radiation therapy. And black men diagnosed with
prostate cancer were 11 percent less likely to get surgical or radiation
treatment.
"It documents the inequities in our society more so than documenting racism
among individual providers," Gross said.
Gross cited other possible factors, including blacks having less access to
quality care due to socioeconomic and other reasons, some blacks being more
likely to have other chronic medical conditions like diabetes that could
complicate cancer therapy, and blacks perhaps being less trusting of the medical
establishment.
Gross said the study did not look at whether there have been improvements since
2002, noting that some initiatives have been put in place since then that might
help close the gap.
(Editing by
Eric Beech)
Racial disparities persist in U.S. cancer treatment, R,
7.1.2008,
http://www.reuters.com/article/domesticNews/idUSN0430653420080107
AIDS
Patients Face Downside of Living Longer
January 6,
2008
The New York Times
By JANE GROSS
CHICAGO —
John Holloway received a diagnosis of AIDS nearly two decades ago, when the
disease was a speedy death sentence and treatment a distant dream.
Yet at 59 he is alive, thanks to a cocktail of drugs that changed the course of
an epidemic. But with longevity has come a host of unexpected medical
conditions, which challenge the prevailing view of AIDS as a manageable, chronic
disease.
Mr. Holloway, who lives in a housing complex designed for the frail elderly,
suffers from complex health problems usually associated with advanced age:
chronic obstructive pulmonary disease, diabetes, kidney failure, a bleeding
ulcer, severe depression, rectal cancer and the lingering effects of a broken
hip.
Those illnesses, more severe than his 84-year-old father’s, are not what Mr.
Holloway expected when lifesaving antiretroviral drugs became the standard of
care in the mid-1990s.
The drugs gave Mr. Holloway back his future.
But at what cost?
That is the question, heretical to some, that is now being voiced by scientists,
doctors and patients encountering a constellation of ailments showing up
prematurely or in disproportionate numbers among the first wave of AIDS
survivors to reach late middle age.
There have been only small, inconclusive studies on the causes of aging-related
health problems among AIDS patients.
Without definitive research, which has just begun, that second wave of suffering
could be a coincidence, although it is hard to find anyone who thinks so.
Instead, experts are coming to believe that the immune system and organs of
long-term survivors took an irreversible beating before the advent of lifesaving
drugs and that those very drugs then produced additional complications because
of their toxicity — a one-two punch.
“The sum total of illnesses can become overwhelming,” said Charles A. Emlet, an
associate professor at the University of Washington at Tacoma and a leading
H.I.V. and aging researcher, who sees new collaborations between specialists
that will improve care.
“AIDS is a very serious disease, but longtime survivors have come to grips with
it,” Dr. Emlet continued, explaining that while some patients experienced
unpleasant side effects from the antiretrovirals, a vast majority found a
cocktail they could tolerate. “Then all of a sudden they are bombarded with a
whole new round of insults, which complicate their medical regime and have the
potential of being life threatening. That undermines their sense of stability
and makes it much more difficult to adjust.”
The graying of the AIDS epidemic has increased interest in the connection
between AIDS and cardiovascular disease, certain cancers, diabetes, osteoporosis
and depression. The number of people 50 and older living with H.I.V., the virus
that causes AIDS, has increased 77 percent from 2001 to 2005, according to the
federal Centers for Disease Control, and they now represent more than a quarter
of all cases in the United States.
The most comprehensive research has come from the AIDS Community Research
Initiative of America, which has studied 1,000 long-term survivors in New York
City, and the Multi-Site AIDS Cohort Study, financed by the National Institutes
of Health, which has followed 2,000 subjects nationwide for the past 25 years.
The Acria study, published in 2006, examined psychological, not medical, issues
and found unusual rates of depression and isolation among older people with
AIDS.
The Multi-Site AIDS Cohort Study, or MACS, will directly examine the
intersection of AIDS and aging over the next five years. Dr. John Phair, a
principal investigator for the study, which has health data from both infected
and uninfected men, said “prolonged survival” coupled with the “naturally
occurring health issues” of old age raised pressing research questions: “Which
health issues are a direct result of aging, which are a direct result of H.I.V.
and what role do H.I.V. meds play?”
The MACS investigators, and other researchers, defend the slow pace of research
as a function of numbers. The first generation of AIDS patients, in the
mid-1980s, had no effective treatments for a decade, and died in overwhelming
numbers, leaving few survivors to study.
Those survivors, like Mr. Holloway, gaunt from chemotherapy and radiation and
mostly housebound, lurch from crisis to crisis. Mr. Holloway says his adjustment
strategy is simple: “Deal with it.” Still he notes, ruefully, that his father
has no medical complaints other than arthritis, failing eyesight and slight
hearing loss.
“I look at how gracefully he’s aged, and I wish I understood what was happening
to my body,” Mr. Holloway said during a recent home visit from his case manager
at the Howard Brown Health Center here, a gay, lesbian and transgender
organization. The case manager, Lisa Katona, could soothe but not inform him.
“Nobody’s sure what causes what,” Ms. Katona told Mr. Holloway. “You folks are
the first to go through this and we’re learning as we go.”
Mr. Holloway is uncomplaining even in the face of pneumonia and a 40-pound
weight loss, both associated with his cancer treatment. Has the cost been too
high? He says it has not, “considering the alternatives.”
Halfway across the country, Jeff, 56-year-old New Yorker who was found to have
AIDS in 1987, said he asks himself that question often.
Jeff, who asked that he not be fully identified, has had one hip replacement
because of a condition called avascular necrosis, the death of cells from
inadequate blood supply, and needs another to avoid a wheelchair. Many experts
think that avascular necrosis is caused by the steroids many early AIDS
sufferers took for pneumonia.
“The virus is under control, and I should be in a state of ecstasy,” he said,
“but I can’t even tie my own shoe laces and get up and down the subway stairs. ”
His bones are spongy from osteoporosis, a disorder that afflicts many
postmenopausal women but rarely middle-aged men, except some with AIDS. No
research has explained the unusual incidence.
In addition, Jeff has Parkinson’s disease, which is causing tremors and memory
lapses.
He is in an AIDS support group at SAGE, a social service agency for older gay
men and lesbians. His fellow group members also say they find the illnesses
associated with age more taxing than the H.I.V. infection. One 69-year-old
member of the group, for example, has had several heart attacks and triple
bypass surgery, and his doctor predicts that heart disease is more likely to
kill him than AIDS.
Cardiovascular disease and diabetes are associated with a condition called
lipodystrophy, which redistributes fat, leaving the face and lower extremities
wasted, the belly distended and the back humped. In addition, lipodystrophy
raises cholesterol levels and causes glucose intolerance, which is especially
dangerous to black people, who are already predisposed to heart disease and
diabetes.
At Rivington House, a residence for AIDS patients on the Lower East Side of
Manhattan, Dr. Sheree Starrett, the medical director, said that neither heart
disease nor diabetes was “terribly hard to treat, except that every time you add
more meds there is more chance of something else going wrong.”
Statins, for instance, which are the drug of choice for high cholesterol, are
bad for people with abnormal liver function, also a greater risk among blacks.
Many AIDS patients have end-stage liver disease, either from intravenous drug
use or alcohol abuse. Among Dr. Starrett’s AIDS patients is 58-year-old Dominga
Montanez, whose first husband died of AIDS and whose second husband is also
infected.
“My liver is acting up, my diabetes is out of control and I fractured my spine”
because of osteoporosis, Ms. Montanez said. “To me, the new things are worse
than the AIDS.”
There are no data that compare the incidence, age of onset and cause of
geriatric diseases in the general population with the long-term survivors of
H.I.V. infection. But physicians and researchers say that they do not see people
in their mid-50s, absent AIDS, with hip replacements associated with vascular
necrosis, heart disease or diabetes related to lipodystrophy, or osteoporosis
without the usual risk factors.
“All we can do right now is make inferences from thing to thing to thing,” said
Dr. Tom Barrett, medical director of Howard Brown. “They might have gotten some
of these diseases anyway. But the rates and the timing, and the association with
certain drugs, makes everyone feel this is a different problem.”
One theory about why research on AIDS and aging has barely begun is “the rapid
increase in numbers,” Dr. Emlet said. The federal disease centers’ most recent
surveillance data, from 33 states that meet certain reporting criteria, showed
that the number of people 50 and older with AIDS or H.I.V. infection was 115,871
in 2005, nearly double the 64,445 in 2001.
Another is the routine exclusion of older people from drug trials by big
pharmaceutical companies. The studies are designed to measure safety and
efficacy but generally not long-term side effects.
Those explanations do not satisfy Larry Kramer, founder of several AIDS advocacy
groups. Mr. Kramer, 73 and a long-term survivor, said he had always suspected
“it was only a matter of time before stuff like this happened” given the potency
of the antiretroviral drugs. “How long will the human body be able to tolerate
that constant bombardment?” he asked. “Well, we are now seeing that many bodies
can’t. Once again, just as we thought we were out of the woods, sort of, we have
good reason again to be really scared.”
The lack of research also limits a patient’s care. Dr. Barrett says the
incidence of osteoporosis warrants routine screening. Medicare, Medicaid and
private insurers, however, will not cover bone density tests for middle-aged
men.
Marty Weinstein, 55 and infected since 1982, has had a pacemaker installed, has
been found to have osteoporosis, and has been treated for anal cancer and
medicated for severe depression — all in the last year. He also has cognitive
deficits.
A former professor of psychology in Chicago, he presses his doctors about cause
and effect. Sometimes they offer a hypothesis, he said, but never a certain
explanation.
“I know the first concern was keeping us alive,” Mr. Weinstein said. “But now
that so many people are going to live longer lives, how are we going to get them
through this emotionally and physically?”
AIDS Patients Face Downside of Living Longer, NYT,
6.1.2008,
http://www.nytimes.com/2008/01/06/health/06HIV.html?hp
In
Global Battle on AIDS, Bush Creates Legacy
January 5,
2008
The New York Times
By SHERYL GAY STOLBERG
WASHINGTON
— Dr. Jean W. Pape did not know what to expect in early January 2003, when he
slipped away from his work treating AIDS patients in Haiti and flew to
Washington for a secret meeting with President Bush.
Mr. Bush was considering devoting billions to combat global AIDS, a public
health initiative unparalleled in size and scope. The deliberations had been
tightly carried out; even the health secretary was left out early on. If
President Bush was going to shock the world — and skeptical Republicans — with a
huge expenditure of American cash to send expensive drugs overseas, he wanted it
to be well spent.
“He said, ‘I will hold you accountable, because this is a big move, this is an
important thing that I’ve been thinking about for a long time,’” recalled Dr.
Pape, one of several international AIDS experts Mr. Bush consulted. “We
indicated to him that our arms are totally broken as physicians, knowing that
there are things we could do if we had the drugs.”
Nearly five years later, the President’s Emergency Plan for AIDS Relief —
Pepfar, for short — may be the most lasting bipartisan accomplishment of the
Bush presidency.
With a year left in office, Mr. Bush confronts an America bitterly split over
the war in Iraq. His domestic achievements, the tax cuts and education reform,
are not fully embraced by Democrats, and his second-term legislative agenda —
revamping Social Security and immigration policy — lies in ruins.
The global AIDS program is a rare exception. So far, roughly 1.4 million AIDS
patients have received lifesaving medicine paid for with American dollars, up
from 50,000 before the initiative. Even Mr. Bush’s most ardent foes, among them
Senator John Kerry of Massachusetts, his 2004 Democratic challenger, find it
difficult to argue with the numbers.
“It’s a good thing that he wanted to spend the money,” said Mr. Kerry, an early
proponent of legislation similar to the plan Mr. Bush adopted. “I think it
represents a tremendous accomplishment for the country.”
Announced in the 2003 State of the Union address, the plan called for $15
billion for AIDS prevention, treatment and care, concentrating on 15 hard-hit
nations in Africa and the Caribbean. An enthusiastic Congress has already
approved $19 billion.
Mr. Bush is pressing for a new five-year commitment of $30 billion. He will
travel to Africa in February to make his case — and, the White House hopes,
burnish the compassionate conservative side of his legacy.
Despite the effort, there are still 33 million people living with H.I.V., and
the United Nations estimates that there were 1.7 million new infections in 2007
in sub-Saharan Africa alone. Critics, including Mr. Kerry, are particularly
incensed by the requirement that one-third of the prevention funds be spent
teaching abstinence, despite a lack of scientific consensus that such programs
reduce the spread of H.I.V.
When a Ugandan AIDS activist, Beatrice Were, denounced the abstinence-only
approach at an international AIDS conference last year, she received a standing
ovation. Paul Zeitz, executive director of the Global AIDS Alliance, an advocacy
group here in Washington, says the Bush program has been hamstrung by
“ideologically driven policies.”
That assessment was echoed, in more diplomatic terms, by the independent
Institute of Medicine, which evaluated the program in March. It called on
Congress to abandon the abstinence requirement and to lift the ban on paying for
clean needles for drug addicts, among other changes.
Yet the institute concluded that, over all, the program had made “a promising
start.” And when they step back, even critics like Mr. Zeitz concede that Mr.
Bush spawned a philosophical revolution. In one striking step, he put to rest
the notion that because patients were poor or uneducated they did not deserve,
or could not be taught to use, medicine that could mean the difference between
life and death.
In Haiti, about 13,000 patients are now receiving anti-retroviral drugs. That is
only half the estimated 26,000 who need them, but far more than the 100 being
treated five years ago. “A huge success story,” Dr. Pape says, “beyond my
imagination.”
In Uganda, a country already far along on its own AIDS initiative when Mr. Bush
began his, 110,000 people are under treatment, and 2 million have H.I.V. tests
each year, up from 10,000 treated and 400,000 tested before, according to Dr.
Alex Coutinho, a top AIDS expert there. The money comes mostly from Pepfar, but
also from a United Nations fund to which the United States contributes.
Dr. Coutinho said Ugandans were terrified that when Mr. Bush left office, “the
Bush fund,” as they call it, would go with him. “When I’ve traveled in the U.S.,
I’m amazed at how little people know about what Pepfar stands for,” he said.
“Just because it has been done under Bush, it is not something the country
should not be proud of.”
The story of how a conservative Republican president became a crusader against
global AIDS is an unlikely one. Mr. Bush ran for the White House in 2000 with
what Joshua B. Bolten, his chief of staff, calls “a Republican’s skepticism
about the efficacy of foreign aid.” He talked of letting “Africa solve Africa’s
problems.” But a variety of forces conspired to put the international AIDS
epidemic on the new president’s agenda.
Colin L. Powell, then the new secretary of state, was deeply troubled by
demographics showing that in some African nations, AIDS threatened to wipe out
the entire child-bearing population — a condition that could create instability,
and a climate ripe for terrorism. Just weeks into his new job, he called Tommy
G. Thompson, the new administration’s health and human services secretary.
“I said, ‘Tommy, this is not just a health matter, this is a national security
matter,’” Mr. Powell recalled. They vowed to work together, and the president,
Mr. Powell said, “bought into it immediately.” Yet, little was done at first,
infuriating advocates like Mr. Zeitz.
By 2002, though, Christian conservatives, a core component of Mr. Bush’s
political base, began adopting the cause. Jesse Helms, the conservative
Republican senator from North Carolina, declared himself ashamed that he had not
done more. Bill Frist, a physician who was then a Republican senator from
Tennessee, was badgering Mr. Bush about the epidemic. So was Bono, the rock
star. Generic drugs were slashing the costs for treatment.
In the spring of that year, Mr. Bush sent Mr. Thompson and the government’s top
AIDS expert, Dr. Anthony S. Fauci, to Africa “to try to scope out anything we
could do in a humanitarian way,” Dr. Fauci said.
They came back and proposed $500 million to prevent mother-to-child transmission
of the disease. The president approved, Dr. Fauci said, but told them to think
bigger.
“He wanted to do something game-changing,” Mr. Bolten said. “Something that,
instead of at the margins assuaging everybody’s conscience, might actually
change the trajectory of this disease which, from the reports we were getting,
was headed to destroy a whole continent.”
Mr. Bolten, Dr. Fauci and a handful of others spent eight months quietly
planning. Inside the White House, Condoleezza Rice, then the national security
adviser, favored the program.
But there was resistance from those who thought it “problematic to be announcing
a lot of money for foreigners,” said Michael J. Gerson, Mr. Bush’s former
speechwriter. Opponents waged an 11th-hour attempt to strip the announcement
from the State of the Union address. Mr. Bush overruled them.
With the United States about to invade Iraq, some theorized that Mr. Bush was
trying to soften the nation’s image. Not so, says Mr. Gerson, who calls the
initiative “foreign policy moralism.” But he does see a link: “It fit a broader
conception of his view of America’s purpose in the world, which included not
just the liberation of other people, but their treatment for disease.”
The goals were ambitious: to treat 2 million people, prevent 7 million new
infections and provide care for 10 million, including orphans and other children
considered at risk, over five years, beginning in 2004 when the money became
available.
The prevention targets will not be measured until 2010. But Dr. Mark Dybul, Mr.
Bush’s global AIDS coordinator, says the program is on track to meet its goals.
In addition to drugs for 1.4 million, the government says it has provided care
for nearly 6.7 million people affected by the disease, including 2.7 million
orphans and other children. Drugs provided to pregnant women have spared an
estimated 152,000 infants from infection, the government says.
Some AIDS experts say the money could be spent more efficiently. Yet the fight
is not over whether to reauthorize the program, but how. Much of the money has
been channeled through American religious-based organizations, drawing criticism
from people like Dr. Coutinho of Uganda, who say local control would cut costs.
Citing the current infection rate, advocates say $50 billion is needed, not $30
billion as Mr. Bush has proposed. Senator Joseph R. Biden Jr. of Delaware, the
Democratic chairman of the Senate Foreign Relations Committee, is also calling
for $50 billion, as is Dr. Coutinho.
“Unless Pepfar is reauthorized at a much higher level,” Dr. Coutinho said, “we
are going to be in the business of playing God.”
At the White House, AIDS advocacy has become a family affair. Laura Bush made
her third trip to Africa last year, and the president’s daughter Jenna
chronicled the life of a young H.I.V.-positive woman in a new book.
Mr. Bush announced his trip to Africa in conjunction with World AIDS Day in
November, quoting from Deuteronomy: “I have set before you life and death ...
Therefore, choose life.”
On that day, the North Portico of the White House was festooned with a huge red
ribbon, the symbol of the fight against the epidemic. Even Mr. Zeitz took it as
a promising sign.
In Global Battle on AIDS, Bush Creates Legacy, NYT,
5.1.2008,
http://www.nytimes.com/2008/01/05/washington/05aids.html?hp
New
H.I.V. Cases Drop, but Rise in Young Gay Men
January 2,
2008
The New York Times
By SARAH KERSHAW
For years
he had numbed his pain and fear with drugs, alcohol and anonymous sex. But in a
flash of clarity one day, when the crystal meth was wearing off, Javier Arriola
dragged himself to a clinic to get an H.I.V. test, years after he stopped using
condoms.
He knew the answer before he received the results, but it was far worse than he
thought: At age 29, he had full-blown AIDS.
He had planned to have a party for his 30th birthday. Instead he was thinking of
hanging himself in his apartment in Hell’s Kitchen.
“There were feelings of terror, like when you were a little kid and there’s that
thing that terrifies you,” he said. “This was it. The worst nightmare, and I
brought this onto myself.”
The number of new H.I.V. infections in men under 30 who have sex with men has
increased sharply in New York City in the last five years, particularly among
blacks and Hispanics, even as AIDS deaths and overall H.I.V. infection rates in
the city have steadily declined.
New figures from the city’s Department of Health and Mental Hygiene show that
the annual number of new infections among black and Hispanic men who have sex
with men rose 34 percent between 2001 and 2006, and rose for all men under 30
who have sex with men by 32 percent.
At a time when the number of new cases among older gay men is dropping — by 22
percent in New York City during the same period — AIDS experts are bearing down
on what they say is a worrisome and perplexing growth of H.I.V. infection among
young men like Mr. Arriola.
So far, they say, the significant factors feeding the trend appear to be higher
rates of drug use among younger men, which can fuel dangerous sex practices,
optimism among them that AIDS can be readily treated, and a growing stigma about
H.I.V. among gays that keeps some men from revealing that they are infected.
There has also been a substantial increase in the number of new infection cases
among young white men who have sex with men, but still that group had fewer new
cases in 2006: 100, compared with 228 among blacks and 165 among Hispanics.
The rising rates for young men in New York City come as federal health officials
acknowledge that infection rates nationwide, while flat, may be substantially
higher than previously thought because of underreporting.
The highest rates of H.I.V. infection nationally are among gays, blacks and
Hispanics, with a recent trend toward a younger infected population mirroring
New York City’s experience, according to AIDS researchers, who say they are
concerned that the country’s infection rates over all have not declined in the
past 10 years.
“It’s really unconscionable that we haven’t had a decrease in new infections in
the past decade in the United States,” said Wafaa El-Sadr, chief of infectious
diseases at Harlem Hospital Center and a professor of public health at Columbia
University. “It’s not anymore in the headlines; many people think it’s gone
away, and it hasn’t gone away.”
AIDS activists and medical providers say the rates among young men could signal
a new wave of the disease.
“Unless you start pulling it apart, unless you start looking at really
addressing this and talking honestly, unless you start talking about it in a
real way,” said Soraya Elcock, deputy director for policy at Harlem United
Community Aids Center, in a neighborhood that has one of the highest infection
rates in the city, “we’ll be here in another 20 years having the same
conversation.”
As a young, black gay man, Lynonell Edmonds says it seems like a miracle that he
has not contracted the AIDS virus. Before he turned 20, he had a haunting
realization: in his group of 20 close gay friends, he was the only one without
H.I.V.
Mr. Edmonds, now 25, does outreach work for the Harlem AIDS center, trolling
Craigslist and other online meeting spots as a “sexpert,” encouraging men to be
tested. He and a crew of outreach workers also go to gay nightclubs late at
night, with a van carrying H.I.V. tests that can be conducted on the spot. The
crew parks the van, which has no obvious signs of its mission, on the street.
When they go into the clubs, they make conversation and delicately inquire
whether a clubgoer would like to take the test.
Mr. Edmonds said that for many gay black men there is a sense that getting the
virus is almost inevitable.
“A lot of guys say, ‘I’m going to get it anyway,’” Mr. Edmonds said.
Mr. Edmonds and other gay men say the stigma of being infected with H.I.V. is
growing, and may be greater now than it was in the 1990s, when the AIDS epidemic
became a unifying cause, a shared tragedy for gay men.
“I call it, ‘Don’t ask, don’t tell,’” Mr. Edmonds said. “People are not asking —
it’s like it’s an offensive question.”
Kyle, who found out that he had the virus two years ago, at the age of 23, said
he had grown weary of what he called “pity dates,” men who agreed to go out with
him after he revealed he was infected, but had no intention of pursuing a
relationship. He said that out of about 10 men he had dated in the last two
years, only one — who was, at 40, the oldest — was willing to go beyond pity
dates.
“They blame you and want nothing to do with you; they put you at the end of the
line,” said Kyle, who spoke on the condition that his last name not be used
because he said he believed his condition would hurt him professionally. “The
older generation sees AIDS as a tragedy, the younger generation sees it as
self-destructive behavior.”
He said he was infected by someone who did not reveal that he had the virus
until after they had unprotected sex.
For Mr. Arriola, who struggled with being molested as a child, the H.I.V.
diagnosis put him at rock bottom, he said.
He continued to use drugs for several more months, but then, as his suicide plan
was becoming an obsession, he called a friend who was a recovering addict. He
got clean and sober, joined a 12-step group, started going to therapy and has
slowly pieced his life back together.
“For me today, I’ve done a lot of work to accept myself. I don’t drink and drug,
I meditate, there’s a lot of visualization of the person I want to be,” he said.
“A lot of it is acceptance. I’m 32, I’m Latin, I’m gay and I have H.I.V. And I
don’t feel bad about it. It’s very, very important for me to not feel shame
about this.”
As the face of the epidemic grows younger, city health officials acknowledge
that their efforts — including a widespread condom distribution program, new
investments in education programs at places including churches, and more
availability of H.I.V. testing — are falling short.
“It leaves us a little bit scratching our heads: What is it that is going on?”
said Christine C. Quinn, the City Council speaker. “Something clearly is not
working, and it’s literally about life or death.”
The city, which has the highest number of AIDS cases in the nation, about
100,000, and one of the highest H.I.V. infection rates, according to the health
department, has made great strides in bringing down H.I.V. rates among
intravenous drug users and pregnant women. The department, which is giving out
three million condoms a month in a program begun last year, has also recently
announced several efforts to expand rapid testing, which provides results within
a day.
The city’s health commissioner, Thomas R. Frieden, said in an interview that the
increasing rates among younger men was being driven by stubbornly high rates of
substance abuse, involving drugs like crystal methamphetamine and cocaine, which
not only reduce inhibitions but can also lead to “hypersexuality”: extended
periods of sexual activity, potentially with multiple partners.
Dr. Frieden also said that another likely explanation was “treatment optimism,”
and the many messages gay men receive through AIDS drug advertisements that
people like Mr. Arriola can live long and normal lives.
“People who grew up watching their friends die of AIDS are a lot more careful
than those who didn’t,” said Dr. Frieden, who said he cared for large numbers of
AIDS patients in his earlier medical practice.
He said the department was planning to begin a new H.I.V. prevention campaign
aimed at younger men, and a new marketing strategy for their condom campaign
later this year. “When’s the last time we saw someone with lesions walking
through Chelsea and Hell’s Kitchen?” said Victoria Sharp, director of the Center
for Comprehensive Care, which is currently providing medical care and other
services to 3,000 H.I.V. patients at Roosevelt Hospital and in Harlem. “You
don’t see it, and we haven’t seen it since the mid-1990s, so there is a whole
generation or two who have grown up without seeing the physical manifestations.”
Health officials said they were also concerned about the growing number of
patients receiving concurrent diagnoses of both H.I.V. and AIDS, after waiting
too long to be tested. And while some policymakers say more aggressive testing
could partly explain the higher infection rates, experts say one in four people
with H.I.V. do not know they are infected, so the actual rates could be much
higher.
Since receiving the AIDS diagnosis, Mr. Arriola, now 32, has developed a large
group of sober friends, become a licensed real estate broker, repainted his
apartment — all things that seemed impossible to imagine in the darkness of his
drug use and when he learned he had the disease.
Then, he said he would look in the mirror and see the worthless person he
believed he was. “I won’t make it to 35,” he would say.
But these days, with the antiviral drugs he takes, about five pills a day, his
health is good, he said. Around his apartment, he has posted upbeat messages to
himself, like the one on his mirror, where he has written “thank you.”
On the refrigerator he has a list of goals: “Write a book, own New York City
property, spread love, own a business (20 million), get a college degree, run a
triathlon, have a family (partner, car with driver and kids) and 190 pounds
(muscle).”
New H.I.V. Cases Drop, but Rise in Young Gay Men, NYT,
2.1.2008,
http://www.nytimes.com/2008/01/02/nyregion/02hiv.html
|