|
Vocapedia >
Health
Medicine, Doctors, Physicians, GPs

How to Tell a Mother Her Child Is Dead
NYT
SEPT. 3, 2016
http://www.nytimes.com/2016/09/04/
opinion/sunday/how-to-tell-a-mother-her-child-is-dead.html

Dr. Cameron Hernandez
of Mount Sinai Hospital's mobile
team
making a house call on
a 96-year-old patient in Manhattan.
Photograph:
Nicole Bengiveno
The New York Times
Bring Back House Calls
NYT
OCT. 14, 2015
https://www.nytimes.com/2015/10/15/
opinion/bring-back-house-calls.html
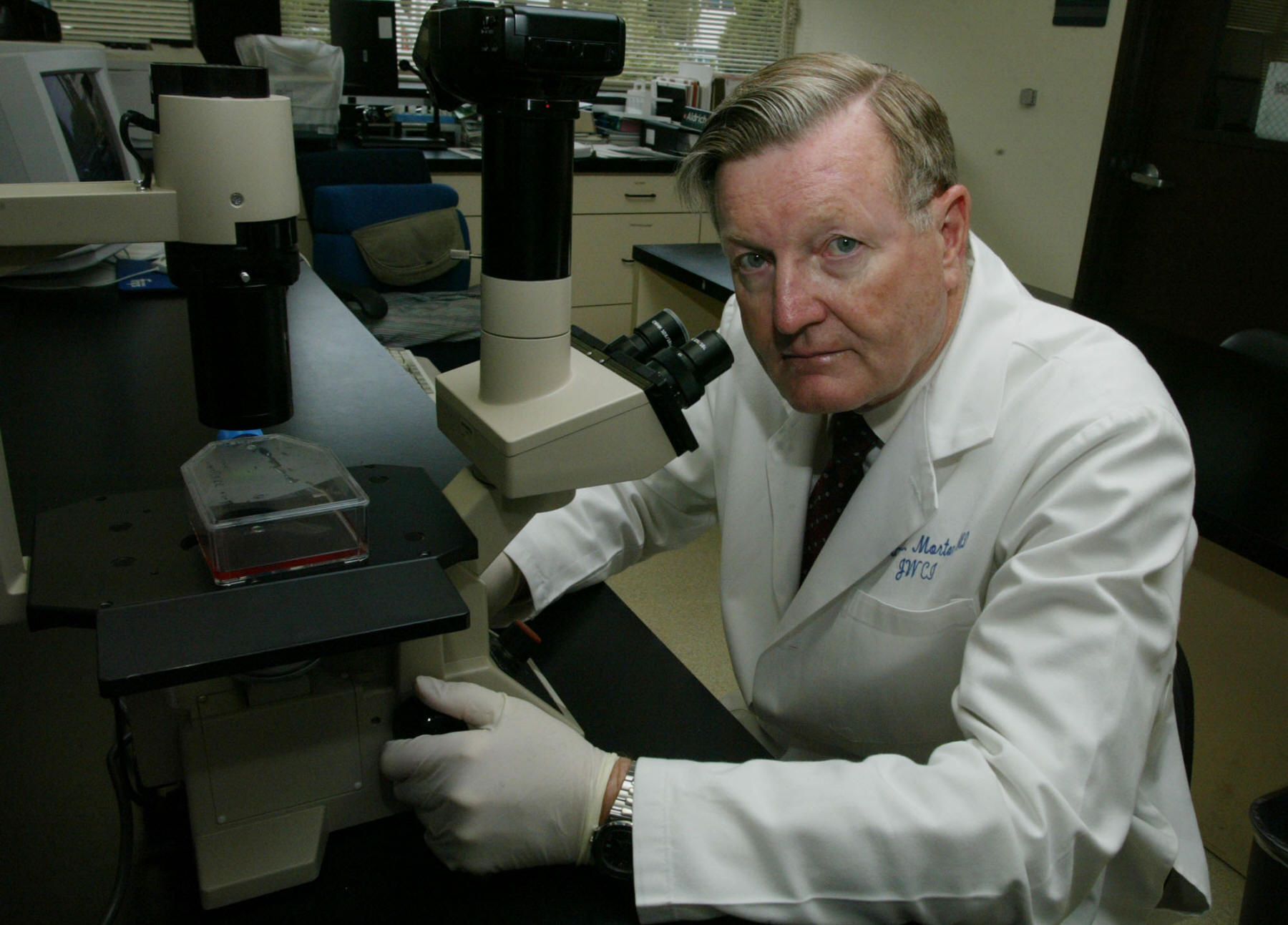
Dr. Donald L. Morton in 2003.
In 1979, he treated John Wayne.
Photograph: J. Emilio Flores
for The New York Times
Dr. Donald Morton,
Melanoma Expert Who Pioneered a Cancer
Technique, Dies at 79
NYT
JAN. 20, 2014
https://www.nytimes.com/2014/01/20/
health/dr-donald-morton-melanoma-expert-who-pioneered-a-cancer-technique-dies-at-79.html

At Beverly Hospital in Bevberly, Massachusetts,
Dr. Timothy
Liesching visits with a patient in via robot
on June 29th, 2009.
Dr. Liesching himself is working
from the Lahey Clinic
in Burlington, Massachusetts,
some 20 miles west.
Photograph: Suzanne Kreiter
Globe staff
The Boston Globe > The Big Picture > More Robots
August 12, 2009
http://www.boston.com/bigpicture/2009/08/more_robots.html - broken link

Country Doctor
Country Dr. Ernest Ceriani
checking blood pressure of
85-year-old Thomas Mitchell
before amputating his gangrenous leg, at hospital.
Location: Kremmling, CO, US
Date taken: August 1948
Photograph:
W. Eugene Smith
Life Images
http://images.google.com/hosted/life/35f6a4a1b73cc17e.html - broken link
General Practitioner GP UK
2022
https://www.theguardian.com/society/2022/nov/27/
stress-exhaustion-1000-patients-a-day-english-gp-nhs-collapse
https://www.theguardian.com/society/2022/feb/22/
my-30-years-as-gp-profession-horribly-eroded-clare-gerada
2021
https://www.theguardian.com/world/2021/jan/13/
gps-in-england-say-inconsistent-supply-of-covid-vaccine-causing-roll-out-issues
2020
https://www.theguardian.com/world/2020/mar/20/
were-clearing-the-decks-a-gp-on-watching-the-coronavirus-pandemic-unfold
2017
https://www.theguardian.com/society/2017/oct/08/
gps-losing-sleep-over-patient-safety-fears-helen-stokes-lampard
2016
http://www.theguardian.com/society/2016/feb/03/
more-than-half-of-gps-say-the-quality-of-their-service-has-deteriorated
2013
http://www.theguardian.com/society/2013/nov/03/
behind-the-scenes-gp-surgery-evenings-weekends
2009
https://www.independent.co.uk/life-style/health-and-families/health-news/
gps-fear-being-sued-in-swine-flu-outbreak-1705507.html - 15 June 2009
2008
http://www.guardian.co.uk/society/2008/feb/10/
health.drugsandalcohol
2007
http://www.theguardian.com/politics/2007/oct/05/
uk.health
GP surgery / GPs' surgeries / doctor's surgery
UK
http://www.theguardian.com/society/2014/apr/13/
gps-surgeries-open-all-hours-50m-pound-reform
http://www.theguardian.com/society/2013/nov/03/
behind-the-scenes-gp-surgery-evenings-weekends
GP / doctor
/ medic UK
https://www.theguardian.com/society/
doctors
https://www.theguardian.com/commentisfree/2018/jun/06/
doctors-mental-health-problems-taboo
https://www.theguardian.com/commentisfree/2017/jul/27/
nhs-doctor-understaffing-patients-at-risk
http://www.guardian.co.uk/society/2010/jun/19/
howard-martin-doctor-euthanasia
http://www.theguardian.com/uk/2006/jun/15/
health.politics
http://www.theguardian.com/society/2005/may/12/
NHS.uknews
General Practitioner GP > country GP >
do rounds UK
https://www.theguardian.com/society/2022/nov/27/
stress-exhaustion-1000-patients-a-day-english-gp-nhs-collapse
NHS doctor
UK
https://www.theguardian.com/society/2018/mar/10/
panic-chronic-anxiety-burnout-doctors-breaking-point
https://www.theguardian.com/commentisfree/2017/jul/27/
nhs-doctor-understaffing-patients-at-risk
NHS junior
doctor UK
https://www.theguardian.com/society/audio/2024/jan/10/
the-uk-government-v-junior-doctors-podcast
https://www.theguardian.com/world/2020/apr/14/
coronavirus-i-worry-about-my-colleagues-
an-nhs-junior-doctor-describes-the-challenges-she-faces
prescription
USA
https://www.npr.org/sections/health-shots/2020/12/15/
946692950/fda-authorizes-first-home-coronavirus-test-
that-doesnt-require-a-prescription
medical
school USA
http://www.npr.org/blogs/health/2015/04/09/
390440465/medical-schools-reboot-for-21st-century
for-profit medical schools
USA
https://www.npr.org/sections/health-shots/2021/06/07/
1002477044/once-banned-for-profit-
medical-schools-are-on-the-rise-again-in-the-u-s
sick leave
UK
http://www.guardian.co.uk/society/2011/nov/19/
sick-leave-independent-assessors-report
USA > doctor / physician
UK, USA
https://www.npr.org/sections/health-shots/2023/08/15/
1193754380/why-doctors-pay-millions-in-fees-that-could-be-spent-on-care
https://www.propublica.org/article/
the-hidden-fee-costing-doctors-millions-every-year - August 14, 2023
https://www.theguardian.com/world/gallery/2023/jul/18/
the-mountain-doctor-on-call-in-north-east-georgia-in-pictures
https://www.nytimes.com/2023/06/15/
magazine/doctors-moral-crises.html
https://www.npr.org/sections/health-shots/2023/03/17/
1164118562/clinics-on-wheels-
bring-doctors-and-dentists-to-health-care-deserts
https://www.nytimes.com/2021/06/03/
health/covid-19-diagnosis-surgeon.html
https://www.npr.org/2020/08/11/
897926271/i-remember-him-with-that-smile-beloved-phoenix-doctor-dies-of-covid-19-at-99
https://www.npr.org/sections/health-shots/2020/06/30/
885186438/a-doctor-confronts-medical-errors-and-flaws-in-the-system-that-create-mistakes
https://www.npr.org/2020/06/26/
883280686/for-hospice-physician-patient-care-means-walking-the-path-with-them
https://www.theguardian.com/artanddesign/2020/may/14/
coronavirus-frontline-hero-rocky-mountain-gp-healed-america-doctors-w-eugene-smith
https://www.nytimes.com/2020/05/02/
opinion/sunday/young-doctor-coronavirus.html
https://www.nytimes.com/2020/04/14/
nyregion/new-york-coronavirus.html
https://www.nytimes.com/2020/04/13/
us/coronavirus-doctor-kirkland-padgett.html
https://www.nytimes.com/2020/03/25/
opinion/coronavirus-doctors-nurses.html
https://www.nytimes.com/2020/03/24/
opinion/coronavirus-hospital-visits.html
https://www.nytimes.com/2020/03/20/
opinion/sunday/coronavirus-hospitals-doctors.html
https://www.npr.org/sections/health-shots/2019/12/30/
786916670/in-rural-areas-without-pain-or-addiction-specialists-family-doctors-fill-in-the-
https://www.npr.org/sections/health-shots/2019/05/31/
728334635/whats-doctor-burnout-costing-america
https://www.npr.org/sections/health-shots/2019/05/21/
725118232/the-struggle-to-hire-and-keep-doctors-in-rural-areas-
means-patients-go-without-c
https://www.npr.org/sections/health-shots/2019/04/26/
717272708/does-taking-time-for-compassion-
make-doctors-better-at-their-jobs
https://www.npr.org/sections/health-shots/2018/07/31/
634217947/to-prevent-doctor-suicides-
medical-industry-rethinks-how-doctors-work
https://www.npr.org/sections/health-shots/2018/01/03/
574701108/brush-with-death-leads-doctor-to-focus-on-patient-perspective
http://www.npr.org/sections/health-shots/2017/07/14/
535792864/doctor-shortage-in-rural-arizona-
sparks-another-crisis-in-forgotten-america
https://www.nytimes.com/2017/06/03/
business/economy/high-end-medical-care.html
http://www.npr.org/sections/health-shots/2017/05/13/
527787511/in-rural-alaska-a-young-doctor-walks-to-his-patients-bedside
http://www.npr.org/sections/thetwo-way/2017/03/10/
519662434/rookie-doctors-will-soon-be-allowed-to-work-up-to-28-hours-straight
http://www.npr.org/sections/health-shots/2017/02/11/
514399475/trump-travel-ban-spotlights-u-s-dependence-on-foreign-born-doctors
http://www.npr.org/sections/health-shots/2017/01/30/
512426568/doctor-considers-the-pitfalls-of-extending-life-and-prolonging-death
http://www.npr.org/sections/health-shots/2016/07/03/
481767273/few-young-doctors-are-training-to-care-for-u-s-elderly
http://www.npr.org/2015/11/08/
448406540/doctor-treats-homebound-patients-often-unseen-even-by-neighbors
http://www.npr.org/sections/health-shots/2015/10/13/
448373459/california-doctors-get-advice-on-how-to-provide-aid-in-dying
http://www.nytimes.com/2015/09/06/
opinion/sunday/a-doctor-at-his-daughters-hospital-bed.html
http://www.nytimes.com/2015/07/26/
opinion/sunday/helping-patients-and-doctors-talk-about-death.html
http://www.nytimes.com/2015/05/17/
opinion/sunday/the-case-for-black-doctors.html
http://www.npr.org/blogs/health/2015/04/09/
390440465/medical-schools-reboot-for-21st-century
http://opinionator.blogs.nytimes.com/2015/02/25/
when-the-system-fails/
http://www.nytimes.com/2015/02/18/
health/doctors-strive-to-do-less-harm-by-inattentive-care.html
http://www.nytimes.com/2014/10/12/
nyregion/to-become-a-doctor.html
http://www.nytimes.com/2014/09/09/
opinion/the-stresses-that-put-doctors-at-risk.html
www.nytimes.com/2014/07/20/
opinion/sunday/bottlenecks-in-training-doctors.html
http://www.nytimes.com/2014/07/20/
opinion/sunday/bottlenecks-in-training-doctors.html
http://www.nytimes.com/2014/02/23/
opinion/sunday/when-doctors-need-to-lie.html
http://www.npr.org/blogs/health/2014/02/04/
271522288/a-denver-family-of-doctors-has-seen-medicine-transformed
http://www.npr.org/blogs/health/2013/12/16/
250194489/how-palliative-care-helps-one-iowa-family-s-experience
http://www.nytimes.com/2013/11/27/
opinion/the-doctor-is-sick-he-will-see-you-now.html
http://www.nytimes.com/2013/11/20/
your-money/how-doctors-die.html
http://www.nytimes.com/2013/11/16/
opinion/sunday/why-doctors-dont-take-sick-days.html
http://www.nytimes.com/2013/10/14/
business/economy/patients-mired-in-costly-credit-from-doctors.html
http://www.nytimes.com/2013/10/06/
opinion/sunday/doctors-bad-habits.html
http://www.nytimes.com/2012/12/16/
opinion/sunday/when-the-doctor-is-not-needed.html
https://www.nytimes.com/2012/08/12/
health/policy/in-ill-doctor-a-surprise-reflection-of-who-picks-assisted-suicide.html
http://www.nytimes.com/2011/09/03/
opinion/when-doctors-become-patients.html
http://www.nytimes.com/2010/05/30/
business/30telemed.html
family doctor
/ physician
USA
https://www.npr.org/sections/health-shots/2019/12/30/
786916670/in-rural-areas-without-pain-or-addiction-specialists-
family-doctors-fill-in-the-
I.C.U.
doctor USA
https://www.nytimes.com/2020/03/24/
opinion/coronavirus-hospital-visits.html
overburdened doctors
USA
https://www.nytimes.com/2022/12/28/
technology/covid-misinformation-online.html
telehealth
doctor USA
http://www.npr.org/sections/health-shots/2017/03/26/
519543337/telehealth-doctor-visits-may-be-handy-but-arent-cheaper-overall
telemedicine consultations USA
https://www.npr.org/sections/health-shots/2018/05/05/
608472248/telemedicine-takes-transgender-care-beyond-the-city
https://www.npr.org/sections/health-shots/2018/01/02/
563736154/can-home-health-visits-help-keep-people-out-of-the-er
http://www.npr.org/sections/health-shots/2017/07/14/
535792864/doctor-shortage-in-rural-arizona-sparks-another-crisis-in-forgotten-america
http://www.nytimes.com/2010/05/30/
business/30telemed.html
remote
medical consultation by videoconference
USA
https://www.npr.org/sections/health-shots/2018/05/05/
608472248/telemedicine-takes-transgender-care-beyond-the-city
virtual
medical appointment USA
https://www.npr.org/sections/health-shots/2020/04/15/
828084250/how-to-get-the-most-out-of-your-virtual-medical-appointment
doctor
shortage
USA
http://www.npr.org/sections/health-shots/2017/07/14/
535792864/doctor-shortage-in-rural-arizona-sparks-another-crisis-in-forgotten-america
rookie
doctors USA
http://www.npr.org/sections/thetwo-way/2017/03/10/
519662434/rookie-doctors-will-soon-be-allowed-to-work-up-to-28-hours-straight
doctors-in-training / interns / trainees / medical residents
USA
https://www.npr.org/sections/health-shots/2019/12/24/
790840216/working-the-christmas-shift-
2-young-doctors-learn-what-it-means-to-be-a-healer
http://www.npr.org/sections/health-shots/2015/12/07/
458049301/is-it-safe-for-medical-residents-to-work-30-hour-shifts
emergency room doctor USA
http://www.nytimes.com/2016/09/04/
opinion/sunday/how-to-tell-a-mother-her-child-is-dead.html
black
doctors USA
http://www.nytimes.com/2015/05/17/
opinion/sunday/the-case-for-black-doctors.html
foreign-born doctors USA
http://www.npr.org/sections/health-shots/2017/02/11/
514399475/trump-travel-ban-spotlights-u-s-dependence-on-foreign-born-doctors
rural
doctor USA
https://www.nytimes.com/2022/09/19/
health/doctor-burnout-west-virginia.html
https://www.npr.org/sections/health-shots/2019/12/30/
786916670/in-rural-areas-without-pain-or-addiction-specialists-
family-doctors-fill-in-the-
http://www.npr.org/sections/health-shots/2017/07/14/
535792864/doctor-shortage-in-rural-arizona-sparks-another-crisis-in-forgotten-america
http://www.npr.org/sections/health-shots/2017/05/13/
527787511/in-rural-alaska-a-young-doctor-walks-to-his-patients-bedside
country doctor
USA
https://www.nytimes.com/2013/02/02/
books/ferrol-sams-doctor-turned-novelist-dies-at-90.html
USA > Georgia > mountain doctor
UK
https://www.theguardian.com/world/gallery/2023/jul/18/
the-mountain-doctor-on-call-in-north-east-georgia-
in-pictures - Guardian pictures gallery
palliative care doctor
USA
http://www.npr.org/sections/health-shots/2016/01/04/
461878689/palliative-care-prepared-for-californias-right-to-die-law-to-take-effect
the waiting room of a doctor’s office
USA
http://www.nytimes.com/2013/10/25/
opinion/getting-to-the-bottom-of-healthcaregovs-flop.html
medical practice / practice
UK
https://www.theguardian.com/society/2022/nov/27/
stress-exhaustion-1000-patients-a-day-english-gp-nhs-collapse
start a
medical practice USA
http://www.nytimes.com/2013/02/02/
books/ferrol-sams-doctor-turned-novelist-dies-at-90.html
cybermedicine / video chat
USA
http://www.npr.org/blogs/alltechconsidered/2015/04/30/
403346731/the-doctor-will-video-chat-with-you-now-insurer-covers-virtual-visits
care
USA
https://www.npr.org/sections/health-shots/2019/05/21/
725118232/the-struggle-to-hire-and-keep-doctors-in-rural-areas-
means-patients-go-without-c
http://www.nytimes.com/2015/02/18/
health/doctors-strive-to-do-less-harm-by-inattentive-care.html
General Medical Council GMC UK
http://www.guardian.co.uk/sport/2009/sep/16/
harlequins-wendy-chapman-bloodgate-gmc
UK > Royal College of General
Practitioners
https://www.rcgp.org.uk/
Donald Lee Morton USA 1934-2014
gained renown as a surgeon
for helping to develop
a widely used technique
for detecting and treating
certain kinds of cancer
http://www.nytimes.com/2014/01/20/
health/dr-donald-morton-melanoma-expert-
who-pioneered-a-cancer-technique-dies-at-79.html
physician USA
https://www.npr.org/sections/health-shots/2019/12/30/
786916670/in-rural-areas-
without-pain-or-addiction-specialists-family-doctors-fill-in-the-
https://www.nytimes.com/2018/02/07/
obituaries/dr-victor-sidel-public-health-champion-is-dead-at-86.html
http://www.npr.org/sections/health-shots/2017/01/30/
512426568/doctor-considers-the-pitfalls-of-extending-life-and-prolonging-death
http://www.npr.org/sections/health-shots/2016/05/24/
479208775/doctor-yearns-for-return-to-time-when-physicians-were-artisans
http://opinionator.blogs.nytimes.com/2015/02/26/
a-mission-of-mercy/
consult a
physician USA
medicine, medicines
The Royal College of Physicians
UK
https://www.rcplondon.ac.uk/
make a house call on N
USA
http://www.nytimes.com/2015/10/15/
opinion/bring-back-house-calls.html
Illustration: Caroline Gamon
When Doctors Need to Lie
NYT
FEB. 22, 2014
http://www.nytimes.com/2014/02/23/
opinion/sunday/when-doctors-need-to-lie.html
specialist
USA
https://www.npr.org/sections/health-shots/2019/12/30/
786916670/in-rural-areas-
without-pain-or-addiction-specialists-family-doctors-fill-in-the-
http://www.nytimes.com/2014/01/19/
health/patients-costs-skyrocket-specialists-incomes-soar.html
addiction specialist
USA
https://www.npr.org/sections/health-shots/2019/12/30/
786916670/in-rural-areas-
without-pain-or-addiction-specialists-family-doctors-fill-in-the-
endocrinologist
USA
http://www.nytimes.com/2012/01/16/
science/wylie-vale-jr-groundbreaking-endocrinologist-dies-at-70.html
urologist
UK
http://www.theguardian.com/education/2015/mar/20/
penis-transplant-surgeon-andre-van-der-merwe-medical-superstar
hepatology
https://en.wikipedia.org/wiki/
Hepatology
hepatologist
UK
https://www.theguardian.com/society/audio/2022/aug/05/
britain-lockdown-drinking-consequences-podcast
dentist UK
https://www.theguardian.com/society/dentists
obstetrics
obstetrician
The Royal College of
Obstetricians and Gynaecologists UK
https://www.rcog.org.uk/
midwife
UK
http://www.guardian.co.uk/lifeandstyle/2010/jul/01/
home-birth-childbirth-babies-study
midwife
pediatrics
paediatrician
USA
https://www.npr.org/sections/health-shots/2022/10/26/
1127393685/why-pediatricians-are-worried-
about-the-end-of-the-federal-covid-emergency
gynaecologist
geriatrics
researcher
surgeon UK
https://www.theguardian.com/uk-news/2017/may/26/
manchester-attack-surgeon-the-impact-for-patients-is-likely-to-be-lifelong
http://www.theguardian.com/commentisfree/2013/dec/20/
abbas-khan-death-syrian-cell-british-surgeon
http://www.theguardian.com/world/2013/dec/18/
syria-foreignpolicy
surgeon USA
http://www.nytimes.com/2016/10/31/
health/dudley-johnson-dead-coronary-bypass.html
http://www.nytimes.com/2015/05/19/
books/review-in-do-no-harm-a-brain-surgeon-tells-all.html
http://www.npr.org/blogs/thetwo-way/2014/01/31/
269380564/brain-surgeon-walks-six-miles-through-storm-to-save-patient
http://www.nytimes.com/2014/01/05/nyregion/
dr-wv-cordice-jr-95-a-surgeon-who-helped-save-dr-king-dies.html
breast cancer surgeon
USA
http://www.nytimes.com/2015/08/10/us/
carolyn-kaelin-breast-cancer-surgeon-dies-at-54.html
heart surgeon
USA
http://www.nytimes.com/2015/04/17/
health/levi-watkins-70-pioneering-heart-surgeon-is-dead.html
surgery
UK
http://www.guardian.co.uk/world/2009/may/01/
dr-john-crippen-swine-flu

Frank Ellis
Picture:
John Redvers
Obituary
Frank Ellis
An oncologist who did much
to further the success
of radiation therapy for
cancer
Christopher Paine
The Guardian
p. 36
Monday February 20, 2006
https://www.theguardian.com/news/2006/feb/20/
guardianobituaries.obituaries1
health care deserts USA
https://www.npr.org/sections/health-shots/2023/03/17/
1164118562/clinics-on-wheels-bring-doctors-and-dentists-to-health-care-deserts
Corpus of news articles
Health > Medicine, Doctors, Physicians,
GPs
Dr.
Richard K. Olney,
Felled
by
the Disease He Studied,
Is Dead
at 64
February 2,
2012
The New York Times
By JOHN SCHWARTZ
Dr. Richard
K. Olney, a leading physician and pioneer in clinical research on amyotrophic
lateral sclerosis, also known as Lou Gehrig’s disease, died of the disease on
Jan. 27 at his home in Corte Madera, Calif. He was 64.
His death was announced by the University of California, San Francisco, where
Dr. Olney had been the director of the A.L.S. Treatment and Research Center
before learning in 2004 that he himself had the disease.
A.L.S. is a degenerative condition of the nerves in the brain and spinal cord
that gradually robs the patient of the ability to use the muscles, trapping the
victim in an increasingly unresponsive body.
Many A.L.S. patients die within two years, but Dr. Olney survived more than
eight after his diagnosis. In that time he was able to see both of his children
get married and to see the birth of his first grandchild, who is named after
him.
“That’s why he lived so long: he was fighting to see those important
milestones,” said Dr. Catherine Lomen-Hoerth, a neurologist who was trained at
the clinic by Dr. Olney, and who took over in 2004 when the illness forced him
to retire. She then directed his care.
Nicholas T. Olney, Dr. Olney’s son, said that his father maintained a
disciplined and upbeat outlook through the course of his illness. “Once he
accepted his diagnosis, he had this attitude that he could make the most of each
day,” he recalled. “He didn’t let the next muscle group, the next ability he
lost, get him down.”
As he explained in an interview with The New York Times in 2005, Dr. Olney first
experienced stiffness in his right leg and loss of coordination in 2003. The
initial diagnosis was a herniated disk. He underwent surgery, but his physical
slide continued.
By May 2005, he had noticed that his right arm was growing stiff and slow. He
then gave himself a common test for A.L.S.: counting the number of times he
could tap his fingers in 10 seconds. He knew that he could normally tap 65
times; he had slowed to 55.
“I knew I had A.L.S. then,” Dr. Olney recalled.
A quiet man, Dr. Olney did not seek publicity until he was struck by the
disease. When he retired from the clinic, he set up an endowment and agreed to
cooperate with journalists in order to build support for the institution. “He
wanted to make sure the A.L.S. center would continue after he was gone,” Dr.
Lomen-Hoerth said.
In a statement, Lucie Bruijn, chief scientist of the A.L.S. Association,
remembered Dr. Olney “not only as a courageous person with A.L.S., but someone
who was an outstanding clinician and scientist who made major contributions both
for patients and the scientific field.”
Richard Knox Olney was born on Dec. 15, 1947, in Munich, to Lt. Col. Frank and
Frances Olney. His family later settled in Norman, Okla. He graduated Phi Beta
Kappa from the University of Oklahoma in 1968 with a bachelor’s degree in
chemistry, mathematics and zoology, and earned a degree in medicine from Baylor
College of Medicine in 1973. He received further medical training at the
University of California, Los Angeles, and the University of Oregon Health
Sciences Center.
At U.C.S.F. he was known as a hard worker whose hours stunned his colleagues.
“He had always told me that the extra time he put in was where he got to do the
fun stuff, like research,” said his son, Nick, who is will begin his medical
residency in neurology this fall.
In addition to his son, Dr. Olney is survived by his wife of 38 years, the
former Paula Louise Zucal; a daughter, Amy Koch Olney Dobbs; his brother, Frank
Jr.; and his grandson.
Dr. Olney and his son were working on a research paper together during his final
months, focused on the use of nerve responses to predict the likely course of
illness in A.L.S. patients. Dr. Lomen-Hoerth will help Nick Olney finish the
paper.
Toward the end, Dr. Olney communicated with the world through a computer that
responded to his eye movements, with the words appearing on a screen.
Since October, his ability to breathe had gradually diminished. But he continued
to send and receive e-mail, and visited the clinic the week before he died to
take part in a research project.
As he got ready to leave, Dr. Lomen-Hoerth recalled: “One of the last things he
tapped out was, ‘goodbye.’ I think he knew it was his last visit.”
“That,” she added, “was a hard thing to see on the screen.”
Dr. Richard K. Olney,
Felled by the Disease He Studied,
Is Dead at 64,
NYT,
2.2.2012,
https://www.nytimes.com/2012/02/03/
us/dr-richard-k-olney-als-researcher-dies-at-64.html
Wylie
Vale Jr.,
Groundbreaking
Endocrinologist,
Dies at 70
January 15,
2012
The New York Times
By NICHOLAS WADE
Wylie W.
Vale Jr., an eminent endocrinologist who helped identify the hormones through
which the brain governs basic bodily functions and who was involved in a
combative race for the Nobel Prize, died on Jan. 3 at his vacation home in Hana,
Hawaii. He was 70.
The cause was not yet known, his wife, Mary Elizabeth, said.
Dr. Vale spent most of his career at the Salk Institute in San Diego, where he
led efforts to identify the group of hormones involved in bodily functions like
growth, reproduction and temperature. Their discovery was a landmark in the
history of endocrinology, coming after more than 30 years of bitter competition.
The Nobel Prize went to others, but Dr. Vale “really, in the long run, had the
biggest impact in the field,” said Bert O’Malley, an endocrinologist at the
Baylor College of Medicine.
The first part of Dr. Vale’s career was spent as the principal scientist in the
laboratory run by Roger Guillemin, who was locked in a 20-year race with a
rival, Andrew Schally, to identify the hormones first.
The Guillemin-Schally war, described by Dr. Schally as “many years of vicious
attacks and bitter retaliation,” ended in a draw in 1977 when the Nobel medicine
committee gave each man a quarter share of a prize, the other half going to Dr.
Rosalyn Yalow.
But the race was not over. An unexpected second phase erupted when Dr. Vale
split from Dr. Guillemin and started competing against his former mentor to find
the remaining hormones.
The serene campus of the Salk Institute, a plaza that overlooks the Pacific
Ocean, then became the home to two laboratories locked in a race for scientific
glory, as Dr. Vale and Dr. Guillemin sought to prove that each could succeed
without the other’s help.
“They sharpened their swords and went at it full bore,” said Ronald Evans, a
hormone expert at the Salk Institute.
Dr. Vale’s first target was the master hormone known as CRF, or corticotrophin
releasing factor, which integrates and controls the body’s response to stress.
Dr. Guillemin and Dr. Schally had spent seven years trying to isolate CRF before
giving up and moving on to easier targets. Dr. Vale discovered CRF in 1981 and
the next year found a second hormone, called the growth hormone releasing
factor, or GRF, which had also eluded the older scientists. GRF controls the
body’s growth.
Endocrinologists watched in amazement as the battle over the hormones raged. But
they let the fight continue, mostly because of the importance of finding the
hormones, but also because the dueling labs had acquired expertise in processing
hundreds of thousands of sheep, pig and beef brains obtained from
slaughterhouses for the research. It was a semi-industrial operation in which
few others cared to join.
Despite the pressure of the competition, first with Dr. Schally and then with
his own mentor, Dr. Vale maintained his easygoing Texan style and sense of
humor. By contrast, Dr. Guillemin, born in Dijon, France, in 1924, brought an
immigrant’s intensity to his work. He was also, like his rival Dr. Schally,
loath to share credit for his lab’s achievements with his younger colleagues.
Toward the end of the fight with Dr. Schally, Dr. Vale became disenchanted with
his mentor’s single-minded quest for scientific renown. During his search for
GRF, Dr. Vale wrote the chemical formula for the hormone — it had not yet been
published — on a large blackboard, which the members of Dr. Guillemin’s lab
could see through the window every morning as they left the Salk parking lot.
The formula was a decoy, intended to mislead the rival team. Dr. Vale kept the
correct version on a piece of paper in his wallet.
Dr. Guillemin was aghast at the challenge from his scientific “son,” a man whom
he had trained for his doctorate. Though he succeeded in finding the CRF and GRF
hormones independently, in both cases Dr. Vale’s lab beat him to the punch.
Wylie Walker Vale Jr. was born in Houston on July 3, 1941. He attended Rice
University and, after hearing Dr. Guillemin lecture on the releasing factors, as
the brain’s hormones are known, joined Dr. Guillemin’s lab at the Baylor College
of Medicine, earning his Ph.D. in 1964.
Dr. Vale’s principal task was to detect the releasing factors’ whereabouts in
the large volumes of tissue from the sheep hypothalamus, a region at the base of
the mammalian brain. He helped Dr. Guillemin to his first success, the
identification of TRF, or thyrotropin releasing factor. Like the other releasing
factor hormones, TRF is produced in the hypothalamus and reaches its target
cells in the pituitary gland, just below the base of the brain. A second
hormone, which is released by the pituitary in response to TRF, controls the
thyroid gland and the body’s temperature control system.
In 1970, Dr. Guillemin moved his team to the Salk Institute. Over the next three
years, Dr. Vale played a central role in the lab’s discovery of LRF, the
releasing factor that controls the whole reproductive system, and somatostatin,
a releasing factor hormone that inhibits the body’s growth.
Dr. Vale founded two companies to exploit his discoveries. One, Neurocrine
Biosciences, is testing drugs that block the action of CRF that may help manage
clinical depression. The other, AcceleronPharma, is testing drugs for treating
anemia.
He also served as president of the American Endocrine Society and was a member
of the National Academy of Sciences.
Besides his wife, who is known as Betty and whom he met in high school in
Houston, Dr. Vale is survived by two daughters, Elizabeth Gandhi and Susannah
Howieson; his father, Wylie; a brother, Shannon; and a granddaughter.
After Dr. Vale’s competition with Dr. Guillemin ended and the two men had
reconciled, Dr. Guillemin recalled how a psychiatrist friend had advised him at
the time to reread the Oedipus myth.
At a tribute on Dr. Vale’s 65th birthday, Dr. Guillemin quoted Freud’s analysis
of the myth: “Part of any son worth his salt is planning the killing of the
father he loves and taking his kingdom.”
Wylie Vale Jr., Groundbreaking Endocrinologist, Dies at 70,
NYT,
15.1.2011,
https://www.nytimes.com/2012/01/16/
science/wylie-vale-jr-groundbreaking-endocrinologist-
dies-at-70.html
Sick leave
should be agreed
by
independent assessors,
says report
Review to recommend taking agreements
over long-term illness benefits
out of hands of
doctors
Saturday 19
November 2011
10.44 GMT
Guardian.co.uk
David Batty
This article was published on guardian.co.uk
at 10.44 GMT
on Saturday 19
November 2011.
It was last modified at 11.24 GMT
on Saturday 19 November 2011.
People should
be signed off for long-term sick leave by an independent assessor rather than
their GP, a government review will recommend.
The independent review, due to be published next week, is also expected to call
for businesses to be given tax breaks for hiring patients with continuing and
unpredictable conditions.
The welfare minister, Lord Freud, said the reforms could lead to "fewer wasted
lives". He said the government wanted to intervene earlier to stop patients
drifting into unnecessary ongoing state support.
A job-finding service to match people with long-term illnesses to suitable work
is expected to be another recommendation of the government-commissioned review.
People who are signed off sick would also be put on to jobseeker's allowance,
rather than employment support allowance, for a period of three months. They
would receive less money and have to prove they were looking for work.
Freud said GPs would still have a role in writing sick notes for up to around
four weeks leave but after that point an independent assessment of the patient's
needs should be carried out.
He told BBC Radio 4's Today programme: "That's the point at which you can get
into drift. If you start having no support at all for the next 28 weeks there's
a very large proportion of people who then drift of into state support and very
long-term support and it's quite unnecessary in many cases."
Freud signalled that the new independent assessment would consider what work
someone seeking long-term sick leave could do and not just consider whether they
were able to continue their current job.
He said: "GPs are not experts necessarily in occupational health and secondly
there's two tests going on – the GP is signing people off for a particular job
but actually in the end the assessment will be when they apply for long-term
state support. The assessment will be 'can you do any job?'. That difference
means that people can fall between the two assessments."
The Independent Review of Sickness Absence, led by Professor Dame Carol Black,
the UK's national director for health and work, and the former head of the
British chambers of commerce David Frost, is looking at ways of cutting the
estimated £60bn cost of working-age ill health.
Black told the BBC: "What the GPs say is they don't have time to do an in-depth
functional assessment and nor have they had any training in occupational health
so we think it's providing a new unique service that both employers and GPs
need."
Frost said when people were off sick for longer than four weeks they started "to
lose the will to work".
"What we've got to do is to find a way of actually working with them,
encouraging them and providing real, practical help. And that's what the
assessment service would do," he told the BBC.
The deputy chair of the British Medical Association's GPs committee, Dr Richard
Vautrey, warned that if the reforms turned out to be "a punitive process just to
try and save money without the best interests of the patient at the heart of the
process then it will fail".
Labour MP Dennis Skinner said: "Last year, the government said GPs should be
accountants in charge of the money that is spent in the NHS. This year they want
assessors to be GPs. It's crazy. No wonder the country is going to the dogs."
The proposed reforms come as the government is embarking on a major and
controversial overhaul of the welfare state. The first independent attempt to
quantify the impact of more stringent medical tests and the greater use of means
testing warned that the tough welfare reforms will force over half a million
people off incapacity benefit and cause widespread poverty in some of Britain's
most disadvantaged communities.
Around 600,000 people would disappear from the benefits system altogether under
changes to be introduced by 2014 and would often have to rely on family members
for financial support, warned researchers from Sheffield Hallam University.
Sick leave should be agreed by independent assessors, says report,
G,19.11.2011,
http://www.guardian.co.uk/society/2011/nov/19/
sick-leave-independent-assessors-report
When
Doctors Become Patients
September
2, 2011
The New York Times
By ERIC D. MANHEIMER
FRANK
SINATRA’S greatest hits album, filtered through the jet engine noise of the
Varian linear accelerator, was not what I felt like hearing at 9 a.m. I made a
mental note to bring a Steely Dan CD for my next appointment.
I was strapped to a hard metal sheet, and the technician had just bolted my head
down using a black mask that had been heat-molded to the contours of my face.
The sheet and I would slide first up and then back in an overhead arc that would
send high-energy electrons into my head and neck from computerized data sets
outlining my throat cancer and its spread into adjacent lymph nodes.
I wasn’t a doctor anymore. I was a patient.
That was almost three years ago. This spring, the Archives of Internal Medicine
published a much-discussed study that showed that doctors might recommend
different treatments for their patients than they would for themselves. They
were far more likely to prescribe for patients a potentially life-saving
treatment with severe side effects than they were to pick that treatment for
themselves.
Understandably, people are worried that this means doctors know something
they’re not telling their patients. But my own experience with illness taught me
a simpler truth: when it comes to their own health, doctors are as irrational as
everyone else.
I had squamous cell carcinoma of the throat, a pea-size lesion first, then the
cancer spread to my lymph nodes. I knew that this was a bad actor; I’d seen the
disease and its consequences many times while wearing a white coat, a
stethoscope dangling from my neck, at a patient’s bedside.
At the beginning, I knew intellectually what was in store for me. I allowed
myself to be a patient, to trust my doctors and let them lead me through the
treatments and complications and side effects that rolled out with alarming
regularity. I submitted to a brutal treatment regimen that had not changed in
over 40 years. Two thousand units of radiation a day for 35 days, with high
doses of platinum chemotherapy, followed, a year later, by a dissection of the
right side of my neck to remove the lymph nodes in which the cancer had
reappeared.
I soon realized I had no idea what kind of rabbit hole I had fallen into.
For my doctors, it was all about the numbers, the staging of my cancer, my loss
of weight and strength. For me, too, it was about the numbers: the six feedings
I pushed through the syringe into the plastic tube in my stomach every day; the
number of steps I could take by myself; how many hours I had to wait before I
could grind up the pill that allowed me to slip into unconsciousness.
But it was also about more: my world progressively shrinking to a small,
sterile, asteroidal universe between the interminable nausea and the chemobrain
that left my head both empty and feverish, between survival and death.
Survival was a percentage, and not a horrible one — 75 percent if I completed
the treatment regimen, by the reckoning of my physicians. But more and more I
found myself thinking about what would happen if I was in that 25 percent. If I
completed the regimen and the tumor came back, there were no other treatment
options. It was morphine and palliative care. I was 58 years old. Death was a
100 percent certainty, eventually. So did it matter?
During one particularly desperate hospitalization, after receiving blood
transfusions and a drug to stimulate my white cells, I decided that I had had
enough. I refused further radiation and chemotherapy. I lay in my bed and
watched the events around me — the distress of my family, the helplessness of my
doctors — without anxiety, comfortable that I had made the correct decision.
My doctors couldn’t override it or persuade me to change my mind, but, luckily,
my wife, Diana, could and did. From my mental cocoon in the hospital bed, I
could sense Diana at my side. “You’re going to finish the treatment,” she said
softly. I did not have the energy, or perhaps the will, to disagree. She wheeled
me down herself to finish my radiation treatments in the basement of the
hospital.
My dreams of dying were not the products of anxious moments of terror. The life
force had simply slipped away and made me ready to die. It had also rendered me
incapable of making the right decision for myself. My disease was treatable and
the odds were favorable. My doctors were professional and gentle but ultimately
could not decide for me. When neither doctor nor patient can make the right
decision, it is vital to have a caring family — though even here the legal and
ethical issues are complicated.
Next week it will be three years since I first noticed the hoarseness that was a
symptom of cancer, and I am back to work and a busy life. But my illness has
changed me profoundly as a physician. Even having lived through this illness,
I’m not sure that I would be any better prepared if I had to relive it again. No
amount of doctoring can prepare you for being a patient.
If anything, it’s that recognition of vulnerability as well as expertise that
makes me a better doctor today.
Eric D. Manheimer,
the medical director of Bellevue Hospital Center,
is the
author of the forthcoming memoir
“Twelve Patients.”
When Doctors Become Patients, NYT, 2.9.2011,
http://www.nytimes.com/2011/09/03/opinion/when-doctors-become-patients.html
The Doctor Will See You Now.
Please Log On
May 28, 2010
The New York Times
By MILT FREUDENHEIM
ONE day last summer, Charlie Martin felt a sharp pain in his lower back. But
he couldn’t jump into his car and rush to the doctor’s office or the emergency
room: Mr. Martin, a crane operator, was working on an oil rig in the South China
Sea off Malaysia.
He could, though, get in touch with a doctor thousands of miles away, via
two-way video. Using an electronic stethoscope that a paramedic on the rig held
in place, Dr. Oscar W. Boultinghouse, an emergency medicine physician in
Houston, listened to Mr. Martin’s heart.
“The extreme pain strongly suggested a kidney stone,” Dr. Boultinghouse said
later. A urinalysis on the rig confirmed the diagnosis, and Mr. Martin flew to
his home in Mississippi for treatment.
Mr. Martin, 32, is now back at work on the same rig, the Courageous, leased by
Shell Oil. He says he is grateful he could discuss his pain by video with the
doctor. “It’s a lot better than trying to describe it on a phone,” Mr. Martin
says.
Dr. Boultinghouse and two colleagues — Michael J. Davis and Glenn G. Hammack—
run NuPhysicia, a start-up company they spun out from the University of Texas in
2007 that specializes in face-to-face telemedicine, connecting doctors and
patients by two-way video.
Spurred by health care trends and technological advances, telemedicine is
growing into a mainstream industry. A fifth of Americans live in places where
primary care physicians are scarce, according to government statistics. That
need is converging with advances that include lower costs for video-conferencing
equipment, more high-speed communications links by satellite, and greater
ability to work securely and dependably over the Internet.
“The technology has improved to the point where the experience of both the
doctor and patient are close to the same as in-person visits, and in some cases
better,” says Dr. Kaveh Safavi, head of global health care for Cisco Systems,
which is supporting trials of its own high-definition video version of
telemedicine in California, Colorado and New Mexico.
The interactive telemedicine business has been growing by almost 10 percent
annually, to more than $500 million in revenue in North America this year,
according to Datamonitor, the market research firm. It is part of the $3.9
billion telemedicine category that includes monitoring devices in homes and
hundreds of health care applications for smartphones.
Christine Chang, a health care technology analyst at Datamonitor’s Ovum unit,
says telemedicine will allow doctors to take better care of larger numbers of
patients. “Some patients will be seen by teleconferencing, some will send
questions by e-mail, others will be monitored” using digitized data on symptoms
or indicators like glucose levels, she says.
Eventually, she predicts, “one patient a day might come into a doctor’s office,
in person.”
Although telemedicine has been around for years, it is gaining traction as never
before. Medicare, Medicaid and other government health programs have been
reimbursing doctors and hospitals that provide care remotely to rural and
underserved areas. Now a growing number of big insurance companies, like the
UnitedHealth Group and several Blue Cross plans, are starting to market
interactive video to large employers. The new federal health care law provides
$1 billion a year to study telemedicine and other innovations.
With the expansion of reimbursement, Americans are on the brink of “a gold rush
of new investment in telemedicine,” says Dr. Bernard A. Harris Jr., managing
partner at Vesalius Ventures, a venture capital firm based in Houston. He has
worked on telemedicine projects since he helped build medical systems for NASA
during his days as an astronaut in the 1990s.
Face-to-face telemedicine technology can be as elaborate as a high-definition
video system, like Cisco’s, that can cost up to hundreds of thousands of
dollars. Or it can be as simple as the Webcams available on many laptops.
NuPhysicia uses equipment in the middle of that range — standard
videoconferencing hookups made by Polycom, a video conferencing company based in
Pleasanton, Calif. Analysts say the setup may cost $30,000 to $45,000 at the
patient’s end — with a suitcase or cart containing scopes and other special
equipment — plus a setup for the doctor that costs far less.
Telemedicine has its skeptics. State regulators at the Texas Medical Board have
raised concerns that doctors might miss an opportunity to pick up subtle medical
indicators when they cannot touch a patient. And while it does not oppose
telemedicine, the American Academy of Family Physicians says patients should
keep in contact with a primary physician who can keep tabs on their health
needs, whether in the virtual or the real world.
“Telemedicine can improve access to care in remote sites and rural areas,” says
Dr. Lori J. Heim, the academy’s president. “But not all visits will take place
between a patient and their primary-care doctor.”
Dr. Boultinghouse dismisses such concerns. “In today’s world, the physical exam
plays less and less of a role,” he says. “We live in the age of imaging.”
ON the rig Courageous, Mr. Martin is part of a crew of 100. Travis G. Fitts Jr.,
vice president for human resources, health, safety and environment at Scorpion
Offshore, which owns the rig, says that examining a worker via two-way video can
be far cheaper in a remote location than flying him to a hospital by helicopter
at $10,000 a trip.
Some rigs have saved $500,000 or more a year, according to NuPhysicia, which has
contracts with 19 oil rigs around the world, including one off Iraq. Dr.
Boultinghouse says the Deepwater Horizon drilling disaster in the Gulf of Mexico
may slow or block new drilling in United States waters, driving the rigs to more
remote locations and adding to demand for telemedicine.
NuPhysicia also offers video medical services to land-based employers with 500
or more workers at a site. The camera connection is an alternative to an
employer’s on-site clinics, typically staffed by a nurse or a physician
assistant.
Mustang Cat, a Houston-based distributor that sells and services Caterpillar
tractors and other earth-moving equipment, signed on with NuPhysicia last year.
“We’ve seen the benefit, ” says Kurt Hanson, general counsel at Mustang, a
family-owned company. Instead of taking a half-day or more off to consult a
doctor, workers can get medical advice on the company’s premises.
NuPhysicia’s business grew out of work that its founders did for the state of
Texas. Mr. Hammack, NuPhysicia’s president, is a former assistant vice president
of the University of Texas Medical Branch at Galveston, where he led development
of the state’s pioneering telemedicine program in state prisons from the
mid-1990s to 2007. Dr. Davis is a cardiologist.
Working with Dr. Boultinghouse, Dr. Davis and other university doctors conducted
more than 600,000 video visits with inmates. Significant improvement was seen in
inmates’ health, including measures of blood pressure and cholesterol, according
to a 2004 report on the system in the Journal of the American Medical
Association.
In March, California officials released a report they had ordered from
NuPhysicia with a plan for making over their state’s prison health care. The
makeover would build on the Texas example by expanding existing telemedicine and
electronic medical record systems and putting the University of California in
charge.
California spends more than $40 a day per inmate for health care, including
expenses for guards who accompany them on visits to outside doctors. NuPhysicia
says that this cost is more than four times the rate in Texas and Georgia, and
almost triple that of New Jersey, where telemedicine is used for mental health
care and some medical specialties.
“Telemedicine makes total sense in prisons,” says Christopher Kosseff, a senior
vice president and head of correctional health care at the University of
Medicine and Dentistry of New Jersey. “It’s a wonderful way of providing ready
access to specialty health care while maintaining public safety.”
Georgia state prisons save an average of $500 in transportation costs and
officers’ pay each time a prisoner can be treated by telemedicine, says Dr.
Edward Bailey, medical director of Georgia correctional health care.
With data supplied by the California Department of Corrections and
Rehabilitation, which commissioned the report, NuPhysicia says the
recommendations could save the state $1.2 billion a year in prisoners’ health
care costs.
Gov. Arnold Schwarzenegger wants the university regents and the State
Legislature to approve the prison health makeover. After lawsuits on behalf of
inmates, federal courts appointed a receiver in 2006 to run prison medical
services. (The state now runs dental and mental health services, with court
monitoring.) Officials hope that by putting university doctors in charge of
prison health, they can persuade the courts to return control to the state.
“We’re going to use the best technology in the world to solve one of our worst
problems — the key is telemedicine,” the governor said.
WITHOUT the blessing of insurers, telemedicine could never gain traction in the
broader population. But many of the nation’s biggest insurers are showing
growing interest in reimbursing doctors for face-to-face video consulting.
Starting in June, the UnitedHealth Group plans to reimburse doctors at Centura
Health, a Colorado hospital system, for using Cisco advanced video to serve
UnitedHealth’s members at several clinics. And the insurer plans a national
rollout of telemedicine programs, including video-equipped booths in retail
clinics in pharmacies and big-box stores, as well as in clinics at large
companies.
“The tide is turning on reimbursement,” says Dr. James Woodburn, vice president
and medical director for telehealth at UnitedHealth.
Both UnitedHealth and WellPoint, which owns 14 Blue Cross plans, are trying
lower-cost Internet Webcam technology, available on many off-the-shelf laptops,
as well as advanced video.
UnitedHealth and Blue Cross plans in Hawaii, Minnesota and western New York are
using a Webcam service provided by American Well, a company based in Boston. And
large self-insured employers like Delta Air Lines and Medtronic, a Blue Cross
Blue Shield customer in Minneapolis, are beginning to sign up.
Delta will offer Webcam consultations with UnitedHealth’s doctor network to more
than 10,000 Minnesota plan members on July 1, says Lynn Zonakis, Delta’s
managing director of health strategy and resources. Within 18 months, Webcam
access will be offered nationally to more than 100,000 Delta plan members.
Dr. Roy Schoenberg, C.E.O. of American Well, says his Webcam service is “in a
completely different domain” than Cisco’s or Polycom’s. “Over the last two
years, we are beginning to see a side branch of telemedicine that some call
online care,” he says. “It connects doctors with patients at home or in their
workplace.”
Doctors “are not going to pay hundreds of thousands of dollars for equipment, so
we have to rely on lower tech,” he adds. The medical records are stored on
secure Web servers behind multiple firewalls, and the servers are audited twice
a year by I.B.M. and other outside computer security companies, Dr. Schoenberg
says.
In Hawaii, more than 2,000 Blue Cross plan members used Webcams to consult
doctors last year, says Laura Lott, a spokeswoman for the Hawaii Medical Service
Association. Minnesota Blue Cross and Blue Shield started a similar Webcam
service across the state last November.
Doctors who use the higher-tech video conferencing technology say that Webcam
images are less clear, and that Webcams cannot accommodate electronic scopes or
provide the zoom-in features available in video conferencing. “If they are not
using commercial-grade video conferencing gear, the quality will be much lower,”
says Vanessa L. McLaughlin, a telemedicine consultant in Vancouver, Wash.
Last month, Charlie Martin, the crane operator, was back in the infirmary of the
Courageous for an eye checkup. In Houston, his face filled the big screen in
NuPhysicia’s office.
After an exchange of greetings, Chris Derrick, the paramedic on the oil rig,
attached an ophthalmological scanner to a scope, pointed it at Mr. Martin’s eye,
and zoomed in.
“Freeze that,” Dr. Boultinghouse ordered, as a close-up of the eye loomed on the
screen. “His eyes have been bothering him. It may be from the wind up there on
the crane.”
The Doctor Will See You
Now. Please Log On,
NYT,
29.5.2010,
https://www.nytimes.com/2010/05/30/
business/30telemed.html
5
Pioneering Scientists
Win Lasker Medical Prizes
September
14, 2008
The New York Times
By LAWRENCE K. ALTMAN
Akira Endo,
a Japanese scientist whose discovery of the first cholesterol-lowering statin
drug helped extend the lives of millions of people, is one of five winners of
this year’s Lasker Awards for medical research, it was announced Saturday.
An American microbiologist, Stanley Falkow of Stanford University, was honored
for greatly expanding knowledge of disease-causing microbes, ranking him as “one
of the greatest microbiologists of all time,” the Albert and Mary Lasker
Foundation said in making the awards.
A third award went to two Americans and a Briton for their pioneering look into
a previously unknown universe of potent molecules, tiny ribonucleic acids known
as micro-RNAs. The Americans are Victor R. Ambros, 54, of the University of
Massachusetts Medical School in Worcester and Gary B. Ruvkun, 56, of
Massachusetts General Hospital in Boston. The Briton is David C. Baulcombe, 56,
of the University of Cambridge.
RNA is DNA’s close chemical cousin. These scientists found that snippets of RNA
act as genetic regulators governing many activities in animals and plants.
Scientists now have implicated micro-RNAs in viral infections, heart failure,
cancer, other diseases, and normal functions like muscle action and blood cell
specialization.
Dr. Endo, 74, was chosen for ushering in a new era in preventing and treating
coronary heart disease, the leading cause of death in the United States and many
other countries, said Dr. Joseph L. Goldstein, chairman of the 24-member
scientific jury that selects the Lasker recipients.
For two years beginning in 1971, Dr. Endo grew more than 6,000 fungi as a
microbiologist working for a Japanese drug company. He was seeking a natural
substance that could block a crucial enzyme involved in the body’s production of
cholesterol, which occurs largely in the liver. Cholesterol is a crucial
component of cells and serves as a raw material for some hormones and nerve
sheaths. But it is also a major contributor to coronary artery disease.
At the time, many scientists were skeptical about the safety of lowering the
amount of cholesterol because it was an essential body chemical. But by 1980,
Dr. Endo’s team found that the statin lowered the LDL, or “bad” cholesterol
level, in the blood by 17 percent.
Dr. Endo went on to identify other statins, and his work led the American
pharmaceutical company Merck to start a program to develop them as drugs.
Merck manufactured lovastatin (Mevacor), the first statin to be licensed, in
1987. Since then, statins have become among the most widely prescribed drugs in
the United States, taken by an estimated 25 million Americans to treat high
levels of LDL cholesterol.
Dr. Falkow, 74, was honored for his discoveries that grew out of an
extraordinary ability to imagine himself as a bacterium so he could view the
world from the microbial perspective.
That talent helped him discover the molecular nature of antibiotic resistance;
forge new laboratory tools that revolutionized the way scientists think about
how microbes cause disease; and train a number of students who have become
scientific leaders in infectious diseases.
Over his 51-year professional career, Dr. Falkow has also developed techniques
to help identify disease-causing bacteria that cannot be grown in the
laboratory; show how bacteria pass certain traits to one another; pave the way
for recombinant DNA technology that has wide use in drug production and in the
laboratory; and help untangle mysteries about how bacteria survive and spread.
Dr. Falkow said his research was conducted at the Walter Reed Army Medical
Center, Georgetown University, the University of Washington and then Stanford.
The three winners in the basic research category were honored for expanding the
versatility of RNA, long regarded as DNA’s poor cousin. Previous scientific
convention held that proteins, not RNAs, governed gene activity in animal cells.
“The notion that small RNAs could control gene expression was unheard of,” said
Dr. Goldstein, the Lasker jury chairman, who works at the University of Texas
Southwestern Medical Center in Dallas.
The scientists’ discovery of micro-RNAs was an accidental finding in research
conducted for other reasons.
Dr. Ambros and Dr. Ruvkun were studying how a roundworm, C. elegans, develops
from newly hatched larva to adult. The worm serves as a model animal for many
geneticists.
Earlier research on flies showed that certain genes instructed embryos where to
place wings, legs and other body parts. Suspecting that other genes specified
the timing of such developmental events, Dr. Ambros focused on lin-4, a gene
that allows immature worms to advance past a particular development stage.
Animals with a defective version of lin-4 cannot pass that hurdle.
Dr. Ambros discovered that animals with a different gene, lin-14, skip early
steps in development and prematurely acquire characteristics that normally
appear later. The two genes exerted opposite effects in worm cells.
Dr. Ambros and Dr. Ruvkun went on to show how the genes collaborated; at an
appropriate time, lin-4 blocks lin-14 activity, allowing worms to continue
normal development.
In a series of additional steps, the researchers found that they were dealing
with very small strands of RNA. At the time, the smallest RNA known to be of
importance in cells consisted of 75 nucleotide building blocks. The RNA they
found was composed of 22 nucleotides.
Dr. Baulcombe, in a seemingly unrelated line of research in England, expanded
the scope of micro-RNAs’ crucial functions by finding that they silenced genes
in plants. He called them silencing RNAs and showed that earlier experiments
were not intended to find micro-RNAs because their size was much smaller than
scientists had imagined.
Now it seems that micro-RNA provides a sophisticated way of adjusting production
of amounts of proteins that are needed at one stage of life but must be absent
in others.
Recent studies suggest that the human genome contains more than 500 micro-RNAs
and that, collectively, they might control a third of all protein-producing
genes. Researchers are now trying to develop drugs that work by blocking
micro-RNAs.
The winners will received their Lasker Awards at a luncheon on Sept. 26. The
prize in each category is $300,000.
5 Pioneering Scientists Win Lasker Medical Prizes,
NYT,
14.9.2008,
https://www.nytimes.com/2008/09/14/
health/14lasker.html
Doctors Wage a Frantic Fight
to Save a Wounded Officer
November 29, 2005
The New York Times
By MICHAEL BRICK
The guarded entrance to Building C of the Kings County
Hospital Center in Brooklyn is designed for ambulance traffic, but the green
Impala that stopped at its painted curb around 3 a.m. yesterday counted as an
emergency vehicle.
There were bullet holes in the doors, and the front-seat passenger, Officer
Dillon Stewart, was bleeding from a massive heart injury.
His wound was severe, but there was cause for hope. Just a few hours earlier,
surgeons at the hospital had opened the chest of a 17-year-old gunshot victim,
saving his life, and now Officer Stewart, 35, was delivering a robust,
thick-walled heart into their care. "The heart has a mind of its own," said Dr.
Robert S. Kurtz, one of his surgeons, "and his was the heart of a fighter."
The fight to keep Officer Stewart alive, which played out over roughly five
hours, was recounted in interviews with Dr. Kurtz and Dr. Patricia O'Neill, the
co-directors of trauma surgery and surgical critical care at Kings County.
Officer Stewart was conscious when he arrived in his unmarked cruiser, but a
slug had crossed through both his left ventricle, the heart's main pumping
chamber, and his left anterior descending coronary artery, which delivers blood
to that ventricle.
Doctors call that a double-hit phenomenon: a glancing blow that leaves two
injuries from the same hole. "I only know of one patient I've treated who
survived it, and that was a knife wound," Dr. O'Neill said. "Bullets do a lot
more damage."
There was no exit wound.
Deep inside Officer Stewart's chest, conflicting forces were at work. His
pericardium, the rigid sack that surrounds the heart, was filling with blood
from the hole in his ventricle. The sack was probably helping keep Officer
Stewart from bleeding to death.
But the blood had to go somewhere. As it filled the sack, it pressed on the
heart, stifling the muscle's ability to pump. Within minutes, the pressure
inside Officer Stewart's chest overwhelmed his cardiac system, and his heart
stopped.
Inside the emergency room, the team of doctors and nurses grew to more than a
dozen. Their patient was now in full cardiac arrest. Pumping medicines, blood
and clotting agents into his veins, they cut open his chest. One of the
surgeons, Dr. L. D. George Angus, took Officer Stewart's heart in his hands,
rubbing it in a gentle clapping motion until it resumed pumping.
To relieve the pressure on the muscle, surgeons cut open the outer sack. But the
bullet wound had to be closed quickly, Dr. Kurtz said, "or he's going to bleed
to death right in front of our eyes."
With a long, narrow pair of metal pliers, Dr. Angus gripped a curved needle and
drew an inch-and-a-half-long blue, nylon-like suture across Officer Stewart's
heart.
Officer Stewart was then taken to a second-floor operating room, where his chest
was sealed.
The surgical team performed transfusions to keep up his blood pressure. They
wrapped his body in a "bear-hugger," a blanket with circulating heat. They
implanted tubes to suck air from his chest.
And their efforts seemed to be working. Their patient's blood pressure was
responding to the treatments. The hole in his artery had clotted. His bleeding
was stanched. The doctors transferred their patient from his stretcher to a bed
in the intensive care unit.
There, Officer Stewart was a room away from his bosses, Mayor Michael R.
Bloomberg and Police Commissioner Raymond W. Kelly, who had arrived and were
waiting with the officer's wife, Leslyn, and other family members.
But behind the door, Officer Stewart went into cardiac arrest a second time.
Surgeons reopened his chest and tried one method after another to restart his
heart. "That's a desperation maneuver, to open his heart in bed in the I.C.U.,"
Dr. Kurtz said.
As Officer Stewart lay there, his heart massaged in a doctor's hands, Mrs.
Stewart was called into the room. "She was muted, traumatized," Dr. Kurtz said.
By 8:40 a.m., her husband would be pronounced dead in his bed in intensive care.
"She had tears in her eyes," Dr. Kurtz said, "and she kissed him."
Doctors Wage a Frantic
Fight to Save a Wounded Officer,
NYT,
29.11.2005,
https://www.nytimes.com/2005/11/29/
nyregion/doctors-wage-a-frantic-fight-
to-save-a-wounded-officer.html
Related > Anglonautes >
Vocapedia
body,
health, medicine, drugs,
viruses, bacteria,
diseases / illnesses,
hygiene, sanitation,
health care / insurance
genetics
mental health, psychology
health,
contraception, abortion,
pregnancy, birth, life,
life expectancy,
getting older / aging,
death
USA > prescription opioid painkillers
lifestyle / health >
exercise,
smoking / tobacco, vaping,
drinking / alcohol,
diet, obesity
Related > Anglonautes >
Science
|